Aspirated Foreign Body
We all have great respect for potential airway disasters. The bouncy ball that lodges in the kids airway leading to respiratory arrest is commonly spoken off and often contemplated. We are ever ready to perform transtracheal ventilation in instances such as this when you cannot oxygenate nor ventilation (see Transtracheal Ventilation and Procedure Videos). Unfortunately, the presentation of an aspirated foreign body is often more subtle than severe.
Severe vs Subtle
- In 2001, ~ 17,537 children < 14 yrs were treated in EDs for choking-related episodes.
- Rates highest for infants (<1 yr) and decreased with age.
- Candy/gum – 19%
- Coins – 12.7%
- In 2000, 160 children < 14 yrs died from aspirated foreign bodies.
- Food substances were involved in 41% of cases.
- Severe symptoms often develop acutely and more commonly have a suspicious history for a aspirated foreign body.
- Cough, stridor, difficulty breathing
- Stupor, cyanosis, respiratory arrest.
- The history, however, may not be helpful in more subtle cases, particularly if the episode was not witnessed or the patient is not able to clearly communicate what happened (ex, infant, debilitated patient, or reluctant / embarrassed teenager).
- The classic presentation of cough, wheeze, and diminished breath sounds are only seen in 40% of patients with aspirated foreign bodies… and when present, can be misconstrued as other conditions like reactive airway disease, URI, or bronchitis.
- Sometimes aspirated foreign bodies can be completely asymptomatic initially and present later with complications of retained foreign body.
- Chronic Cough
- Recurrent pneumonia
- Recurrent / persistent “croup”
- Poorly controlled “asthma”
- Lung abscess
- Hemoptysis
- Progressive respiratory distress
- Death
If you are considering the diagnosis of chronic cough or recurrent pneumonia, high on your potential DDx should be undiagnosed retained foreign body.
Tracheal vs Bronchial Foreign Body
- Patients with a tracheal foreign body are more likely to have:
- Dyspnea.
- Early diagnosis compared to bronchial foreign bodies.
- Patients with a bronchial foreign body are more likely to have:
- Alternative diagnosis upon first presentation.
- Delayed Diagnosis.
- Decreased breath sounds.
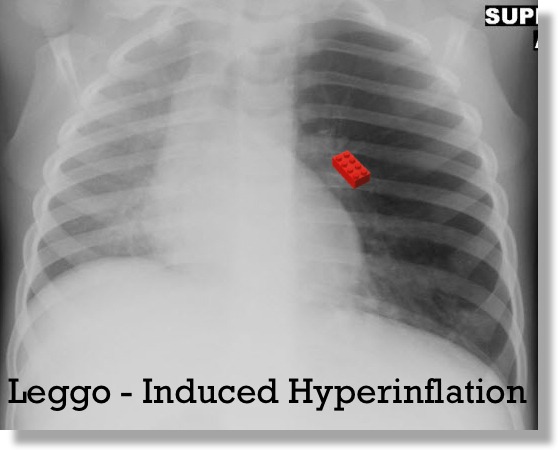
Plain Radiograph Utility
- Unfortunately, plain x-rays are not adequate enough to rule-out the presence of a aspirated foreign body.
- One study that compared radiographic findings to endoscopic findings found no abnormalities on x-ray in 24% of confirmed foreign body cases.
- Their sensitivity and specificity were 68% and 67% respectively.
- As with all testing, your pre-test probability needs to be factored into the interpretation of the results.
The parents saw the child put a Leggo piece in his/her mouth and now that piece is missing and the kid has a persistent cough: a normal x-ray does not take the possibility of aspirated foreign body off of the DDx.
The Evaluation
- Naturally, based on the above, a high index of suspicion is necessary in many cases of aspirated foreign body that present less acutely.
- For those in acute distress, support oxygenation and ventilation!
- For others, obtain plain films with the understanding of their limitations.
- Look for focal hyperinflation
- May need exhalation film (for kid who cooperates)
- May need decubitus film (for younger kid) – the dependent lung should not be normal size… if it is, it is hyperinflated.
- Focal atelectasis may also be present.
- Look for focal hyperinflation
- CT Scanning may reveal material in the airway and focal airway edema, but comes with cost of radiation, and does not offer therapeutic option if foreign body present. CT may also not show rule out all foreign bodies.
- Bronchoscopy is the preferred Diagnostic and Therapeutic plan.
- Flexible Bronchoscopy may be used to define and detect the foreign body, but removal of the foreign body is often more difficult with the flexible scope.
- Rigid Bronchoscopy is the the preferred procedure for removal of the foreign body.
Center for Disease Control Morbidity and Mortality Weekly Report. Nonfatal choking-related episodes among children – United States, 2001. Oct 25, 2002; 51(42): 945 – 948.
Svedstrom E, Puhakka H, Kero P. How accurate is radiography in the diagnosis of tracheobronchial foreign bodies in children? Pediatr Radiol. 1989; 19(8): 520 – 522.
Saki N, Nikakhlagh S, Rahim F, Abshirini H. Foreign body aspirations in infancy: a 20-year experience. International Journal of Medical Sciences. 2009; 6(6): 322 – 328.


[…] Peds EM Morsels […]
[…] have discussed many topics with respect to the pediatric foreign body (Aspirated FB, Nasal FB, Button Batteries in the nose, Esophageal Button Batteries), but let us look at the other […]