Coarctation of the Aorta in Older Children
We have discussed my philosophy of pediatric EM prior: primarily it is composed of a wide variety of “grandma diagnoses,” that can be accurately diagnosed and managed by an astute grandmother. Our purpose, however, is to not be another “grandma,” but rather ensure that grandmothers are not missing more considerable conditions. For instance, you are trained to pick up on the inborn of metabolism amongst all of the children of vomiting. It is a tough job, certainly, but occasionally, some of those less common conditions present to us and their diagnosis is made just by your simple consideration of its possibility: “you can’t diagnose it if you don’t think about it.” This week, we had such an event occur.
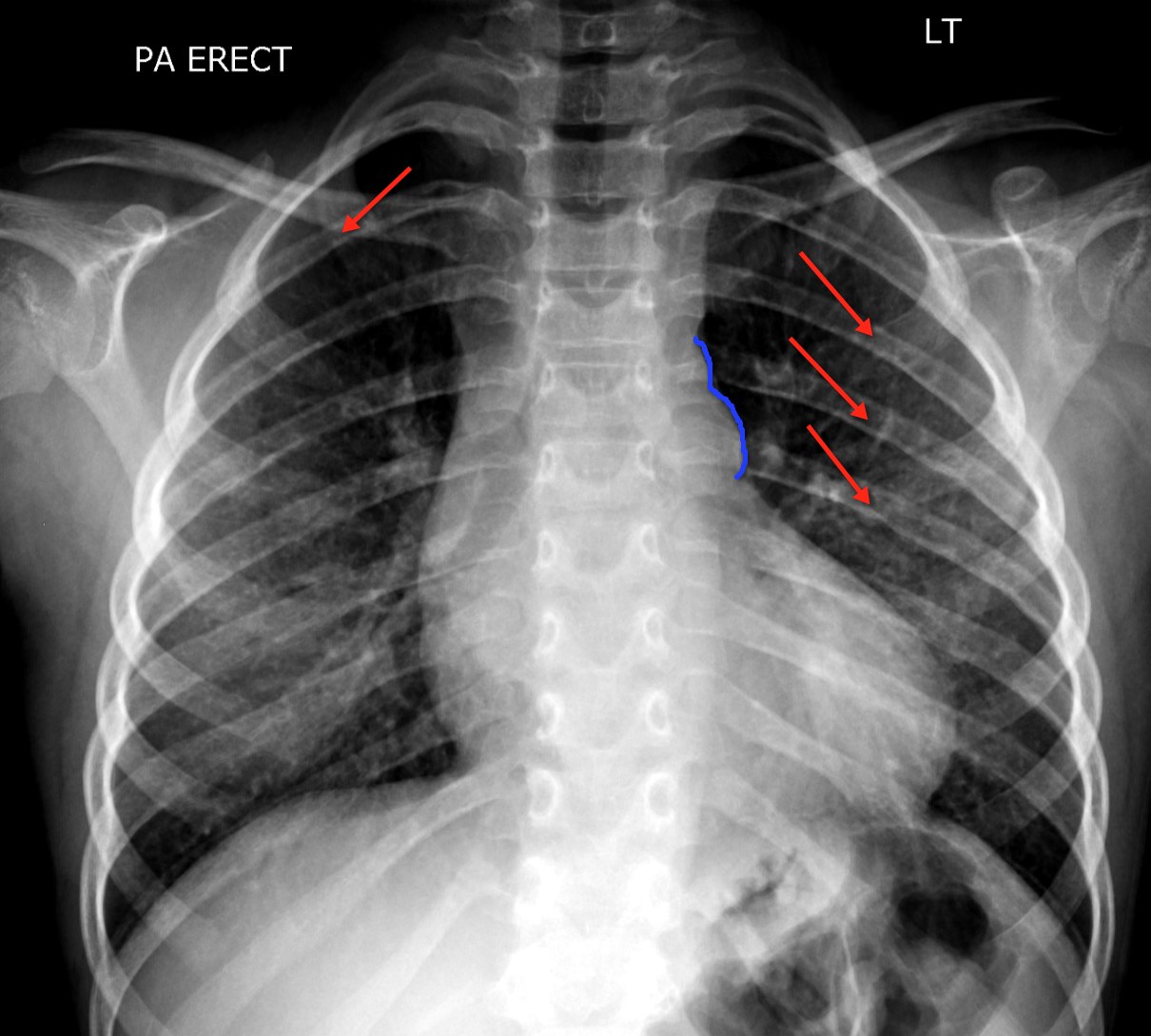
6 yo female presents for maternal concern of high blood pressure. It was noted during routine exam ~1month ago and being “monitored.” Mother became concerned when she found the SBP >150. Child has otherwise been fine. No edema noted. No fevers. No exercise intolerance. The urinalysis was normal. The renal function normal. There was a loud systolic murmur and diminished femoral pulses. CXR was classic with it’s abnormalities (see website). Cardiology agreed to perform ECHO, which demonstrated critical coarctation of the aorta. Nothing against grandma, but I think this family was glad they came to see us in the Peds ED.
a) Coarctation of the Aorta Background
i) Accounts for ~7% of all live births with congenital heart disease
ii) Significant association with other cardiac lesions
(1) VSD, PDA
(2) 50% will have bicuspid aortic valve
iii) Most are diagnosed within the first year of life
(1) Always consider in the neonate who becomes critically ill, acidotic, and/or with poor perfusion to lower extremities.
(2) Critical coarctations can present as the ductus arterious closes leading to restricted blood flow to lower body.
b) Coarctation presenting in later childhood
i) While the presentation in the first year of life can be rather dramatic (heart failure, circulatory collapse, death – all dramatic things), later in life the presentation can be more insidious and can go overlooked or underappreciated.
(1) Systolic murmur (often conducted to back)
(2) Weak or absent femoral pulses (radio-femoral delay in older patients)
(3) Upper limb hypertension
(4) Exercise intolerance
(5) Leg claudication
ii) Certainly, if undiagnosed and severe, coarctation can still produce significant morbidity and mortality (and is why we need to diagnosis it)
(1) Dysrhythmias
(2) Heart Failure
(3) Intracranial hemorrhage
(4) Aortic dissection
(5) Infective endocarditis
(6) Death
c) Clinical Diagnosis
(1) Murmur
(2) Upper limb hypertension
(3) Diminished or absent femoral pulses
d) CXR finding
i) Rib notching (see red arrows on xray)
(1) Best sign in older patients
(2) Due to collateral blood vessels
ii) Figure “3” sign (see blue line)
(1) Seen in ~50% of patients with coarct.
(2) Abnormal aortic knob shadow from coarct and dilation of the left subclavian artery.
So, while this may not be a diagnosis seen every day, it is one that should be considered on your differential of that child with hypertension or murmur… and shock too.
References:
- Rosenthal E. Coarctation of the aorta form fetus to adult: curable condition or life long disease process? Heart Nov 2005; 91(11): 1495-1502
- Strafford MA, Griffiths Sp, Gersony WM. Coarctation of the Aorta: A Study in Delayed Detection. Pediatrics 1982; 69(2): 159-163.
- LearningRadiology.com