Lisfranc Injuries in Pediatric Patients
Spring is coming, and with good weather comes kids playing outside… and broken bones. We have previously discussed ankle injuries, shoulder dislocations, wrist fractures, and even toddler’s fractures. These are all quite common. So let’s step into the realm of the less common, and jump on a rare but easily missed injury- the Lisfranc injury:
Pediatric Lisfranc Injuries: Basics
- Lisfranc JOINT is the tarsometatarsal joint [Cadogan 2022]
- Lisfranc LIGAMENT connects superolateral surface of medial cuneiform to superomedial surface of base of 2nd metatarsal [Cadogan 2022]
- Lisfranc INJURY caused by a direct blow to the foot after jump or fall from height, or forced dorsiflexion flexion with rotational force [Johnson M 2022]
- Known as the “bunk bed fracture” [Johnson G 1981]
- UNCOMMON injury in children. [Gill 2018]
- One of largest case series included only 18 children. [Johnson M 2022, Wiley 1981]
- Hill et al reviewed 56 injuries over a 12 year period [Hill 2017]
- Youngest reported cases were 1-3 years old. Mostly an injury of older children. [Kay 2001, Johnson G 1981]

Pediatric Lisfranc Injuries: Presentations
- Presentations can be mild with pain and swelling at the base of the first and second metatarsal [Johnson M 2022]
- Can be severe with swelling and bruising on the plantar surface of the foot [Johnson M 2022]
- Test by holding the hindfoot fixed and applying abduction and pronation of the forefoot to cause pain. [Johnson M 2022]
Pediatric Lisfranc Injuries: Types
[Johnson M 2022, Queno 1901]
- Type A: total incongruity of the metatarsal joint in a single plane
- Type B: partial incongruity of the metatarsal joint with medial displacement of the first metatarsal OR lateral displacement of the lateral metatarsals. **Most common type in children.
- Type C: divergent pattern with the first metatarsal displaced medially and the lateral metatarsals displaced laterally
Pediatric Lisfranc Injuries: Imaging
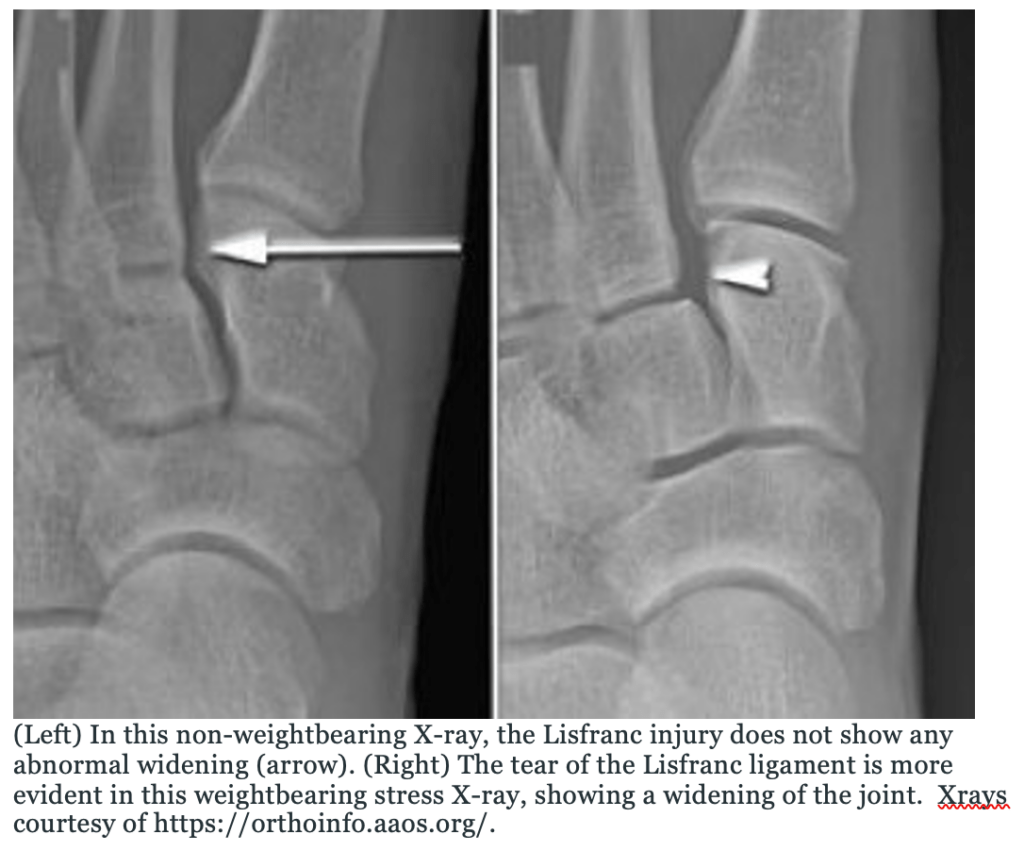
- Weightbearing views are needed. Can be missed on non-weightbearing films. [Johnson M 2022, Crawford 2010]
- AP, Lateral, and Oblique views
- AP films:
- Lateral border of the 1st metatarsal should align with lateral border of medial cuneiform.
- Medial border of the 2nd metatarsal should align with medial border of middle cuneiform
- Oblique films:
- Medial border of 4th metatarsal should align with medial border of cuboid.
- Disruption of lines or diastasis >2mm between base of 1st and 2nd metatarsals indicates Lisfranc injury
- AP films:
Pediatric Lisfranc Injuries: Management
- <2mm displacement
- Place in bulky dressing or well-padded splint/ short leg cast until swelling improves.
- Nonweightbearing in a short leg cast for 4-6 weeks [Kay 2001, Crawford 2010, Wiley 1981]
- Some recommend short leg walking cast 4-6 weeks until pain and tenderness resolve [Buoncristiani 2001]
- >2mm displacement [Johnson M 2022]
- Operative management needed
- Closed reduction with percutaneous pinning if possible [Kay 2001]
- Open reduction internal fixation (ORIF) if closed anatomic reduction not possible [Kay 2001]
Pediatric Lisfranc Injuries: Complications
[Crawford 2010, Wiley 1981, Buoncristiani 2001]
- Pain from posttraumatic arthritis from missed injury
- May have loss of reduction or non-anatomic reduction
- May need arthrodesis if prolonged injury and pain
- Physeal arrest [Hill 2017]
Moral of the Morsel
- Lisfranc injuries are rare in children, and easy to miss. Be vigilant for a concerning mechanism, especially when falling from a bunk bed!
- Weightbearing Xray views are often needed.
- Treatment may be nonoperative if minimal or no displacement, otherwise surgical management needed.
References:
Cadogan M, Gomez A. Jacques Lisfranc. Life in the Fast Lane • LITFL. https://litfl.com/jacques-lisfranc/#:~:text=Jacques%20Lisfranc%20de%20Saint%2DMartin,amputation%20of%20the%20cervix%20uteri. Published 2022. Accessed March 18, 2022.
Johnson M, Riccio A. Foot Dislocations (Lisfranc and Subtalar) | Pediatric Orthopaedic Society of North America (POSNA). Posna.org. https://posna.org/Physician-Education/Study-Guide/Foot-Dislocations-(Lisfranc,Subtalar). Published 2022. Accessed March 18, 2022.
Johnson G. Pediatric Lisfranc injury: “bunk bed” fracture. American Journal of Roentgenology. 1981;137(5):1041-1044. doi:10.2214/ajr.137.5.1041
Gill LE, Klingele KE. Management of foot and ankle injuries in pediatric and adolescent athletes: a narrative review. Orthop Res Rev. 2018;10:19-30
Wiley JJ. Tarso-metatarsal joint injuries in children. Journal of Pediatric Orthopaedics. 1981;1(3):255–260.

