Pediatric Sepsis Definition 2024
Traveling Ticks: Tickborne Illnesses and International Travel
Rebaked: Inborn Errors of Metabolism presenting in the ED
Kounis Syndrome

Gelastic Seizures: No Laughing Matter
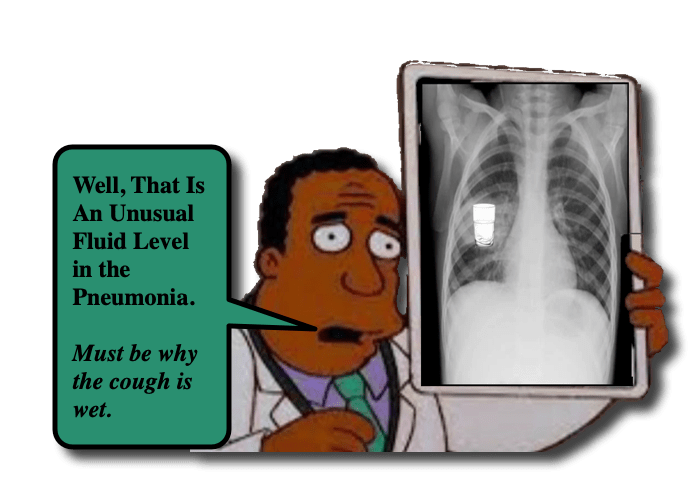
Lung Abscess in Children

Travel-Related Illnesses in Children
Pseudoparalysis of Parrot

Cuffed Endotracheal Tubes for Children: ReBaked Morsel
Imported Malaria