Lung Abscess in Children
We have digested many Morsels regarding various pulmonary complaints. While some are very rare (ex, Pulmonary Embolism, Pulmonary Hypertensive Crisis, Negative Pressure Pulmonary Edema, CPAM) others are commonly encountered (ex, Croup, Bronchiolitis, Sinusitis). It is pneumonia, however, that often generates the most conversations. When should I consider a CXR? What antibiotics are appropriate? Why does this infiltrate appear round? Why does this pneumonia keep recurring? Sure, most pneumonia’s are pretty strait forward, but ever so often they can also become complicated. We’d discussed parapneumonic effusions in the past and now, let’s consider another complication – Lung Abscess in Children:
Lung Abscess in Children: Basics
- Parapneumonic fluid collections occur in up to 40% of children with Bacterial Pneumonia.
- Lung abscess is a rare subset of these (< 1% of admitted cases of pneumonia (Wojsyk-Banaszak, 2018)
- Lung abscess = collection of fluid within a thick-walled localized area of necrotic lung parenchyma. (Wojsyk-Banaszak, 2018; Kraft, 2018)
- Primary vs Secondary Lung Abscesses (Fernando, 2022)
- Primary
- Most common
- No underlying lung disease / abnormal anatomy
- Typically caused by:
- Streptococcus pneumoniae, Staphylococcus aureus, and Oral bacteria
- May be polymicrobial
- Secondary
- Underlying structural or functional pulmonary disease
- May be congenital (ex, Immunodeficiency)
- May be acquired (ex, Aspiration)
- May be caused by similar organisms as primary, but also commonly caused by Gram-Negative Bacteria (like Pseudomonas aerugingsa).
- Patients with immunocompromised conditions are at risk of Fungal infections.
- A complicated primary lung abscess, may develop enough structural destruction that then allows for a secondary lung abscess to occur also. (Matsushima, 2023)
- Underlying structural or functional pulmonary disease
- Primary
- While lung abscess is a severe complication, most children recover without long-term pulmonary sequelae (Wojsyk-Banaszak, 2018)
Lung Abscess in Children: Presentation
- Clinically (Wojsyk-Banaszak, 2018; Kraft, 2018)
- Prolonged cough
- Fever (97.9%)
- Tachypnea (49%)
- Night sweats
- Pleuritic Chest Pain (32.6%)
- Abdominal Pain (22.4%)
- Hemoptysis (sometimes)
- Radiographically
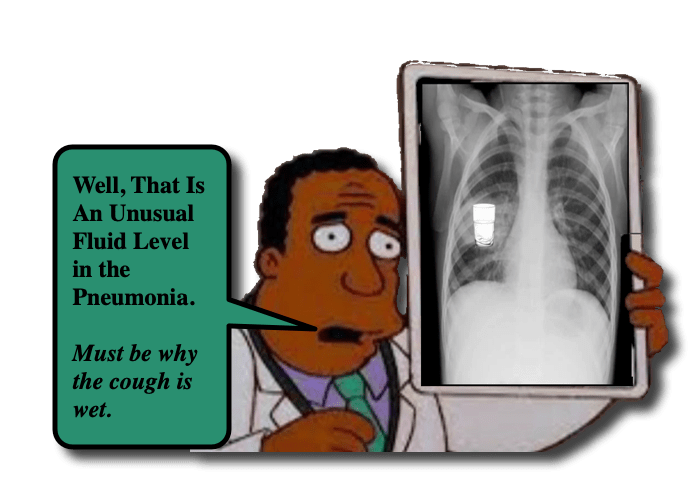
- Chest X-Ray – possible air/fluid level
- Ultrasound (Wojsyk-Banaszak, 2018; Kraft, 2018)
- May be more sensitive than CXR (Kraft, 2018)
- Can show pleural thickening, subpleural consolidation, and B-line artifacts.
- Chest CT
- Demonstrates parenchymal disease better
- Allows for operative planning (if needed)
Lung Abscess in Children: Management
- Rarity of the condition affects what is known (no randomized control trials on therapeutic options). (Wojsyk-Banaszak, 2018)
- Mainstay of initial therapeutic management is: (Wojsyk-Banaszak, 2018; Fernando, 2022)
- Prolonged course of IV antibiotics
- Chest physiotherapy
- Patients managed with medical strategies (compared to surgical) had lower complication rates and shorter hospitalizations.
- May require drainage: (Fernando, 2022)
- Pigtail Catheter inserted under CT-guidance
- Surgical thoracotomy
- Video-Assisted Thoracoscopic Surgery (VATS)
- There is known variability of both selection of antibiotics and management of lung abscess in children (Fernando, 2022)
- A Proposed Algorithm (Fernando, 2022) highlights importance of IV Antibiotics and Chest Physiotherapy for Primary Lung Abscess
- If Secondary Abscess, management is directed toward that underlying condition.
- If Fever resolves with IV antibiotics, then patient will need to complete 4-6 week course.
- If Fever is not resolved (by 48 hrs?), then consider empyema and need for drainage.
- If patient clinically deteriorates / no response to prior therapies, then that is when VATS or open procedure would be considered.
Moral of the Morsel
- Simple things can become Complicated. Life, after all, is complex.
- Lungs do not like Fluid. Scrutinize that CXR for an Air-Fluid Level… and maybe use your Ultrasound to increase your sensitivity!!
- Not all abscesses need to be drained in order to resolve. While drainage may be required, IV antibiotics and optimal medical care is the primary management strategy for lung abscess in children.
References:
Matsushima A, Mizuno S, Minamikawa S, Nakagishi Y, Kasai M. Pneumococcal pneumonia complicated by Aspergillus fumigatus and Pseudomonas aeruginosa lung abscesses. Pediatr Pulmonol. 2024 Jan 11. doi: 10.1002/ppul.26854. Epub ahead of print. PMID: 38206051.
Fernando DT, Bhatt R, Saiganesh A, Schultz A, Gera P. Lung abscess: 14 years of experience in a tertiary paediatric hospital. ANZ J Surg. 2022 Jul;92(7-8):1850-1855. doi: 10.1111/ans.17844. Epub 2022 Jun 9. PMID: 35678219.
Wojsyk-Banaszak I, Krenke K, Jończyk-Potoczna K, Ksepko K, Wielebska A, Mikoś M, Bręborowicz A. Long-term sequelae after lung abscess in children – Two tertiary centers’ experience. J Infect Chemother. 2018 May;24(5):376-382. doi: 10.1016/j.jiac.2017.12.020. Epub 2018 Feb 15. PMID: 29454633.
Kraft C, Lasure B, Sharon M, Patel P, Minardi J. Pediatric Lung Abscess: Immediate Diagnosis by Point-of-Care Ultrasound. Pediatr Emerg Care. 2018 Jun;34(6):447-449. doi: 10.1097/PEC.0000000000001547. PMID: 29851922.

