Congenital Pulmonary Airway Malformation (CPAM)
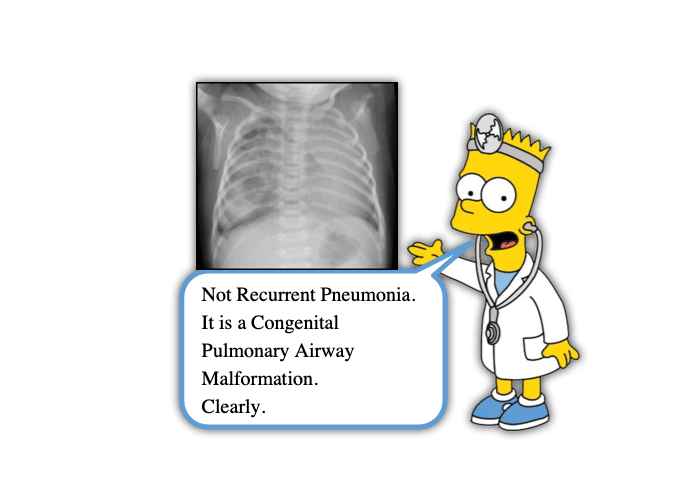
I’m sure you can recall at least several parents who bring their children into the ED for concern of recurrent pneumonias. Often the parents focus on a possible underlying immunodeficiency. Fortunately, most commonly these pneumonias are due to viral infections, and we can often offer reassurances to the parent. The differential could also include aspiration, asthma, and bronchiectasis depending on the patient’s history. There is another item on the differential list that we often don’t think about – structural anomalies. Congenital Pulmonary Airway Malformation (yes, it’s a mouthful just like a delicious PEM morsel) falls into this latter category. This is also referred to as Congenital Cystic Adenomatoid Malformation (CCAM) – an even bigger mouthful. Let’s take a moment to digest a morsel on this condition that may lead to recurrent pulmonary problems:
Congenital Pulmonary Airway Malformation: Basics
- Developmental lesion of the lungs characterized by pseudocysts, lesions, and dilated airways (Dessole, 2019)
- Incidence is 1 in 11,000 to 1 in 35,000 (Dessole, 2019)
- Most often unilateral
- 85% are diagnosed prenatally on ultrasound which is why we don’t often think about it in the ED (Leblanc, 2017)
- Accounts for 95% of congenital cystic lung diseases (David, 2016)
- Commonly misdiagnosed as pulmonary cyst, pulmonary bullae or pneumothorax on Xray (Zhang, 2015)
Congenital Pulmonary Airway Malformation: Presentation & Evaluation
- Cough is the most common presenting complaint followed by breathing difficulty, fever, acute respiratory distress, failure to thrive, and recurrent pneumonias (Mehta, 2016)
- In 50% of cases not diagnosed before birth, CXR shows a hyperlucent mass with occasional radio-opaque components (Leblanc, 2017)
- CT Angio of the chest can detect nearly 100% of cases, but they will often still need a tissue sample for diagnosis (Leblanc, 2017)
- Complications include mediastinal shifts, tracheal deviation, pneumothoracies, pulmonary hemorrhage, nutritional difficulties, and sudden respiratory distress (Leblanc, 2017)
- Can evolve to Pleuro-Pulmonary Blastoma (PPB) and Bronchio-Alveolar carcinoma (BAC) (David, 2016)
- Fatalities are rare but a recent case report has shown CPAM to be linked with sudden infant death from large pneumothorax development (Salerno, 2022)
Congenital Pulmonary Airway Malformation: Management
- Infants are managed expectantly at birth as some of these lesions simply disappear (Mafalda, 2016)
- Symptoms can appear at any age with the median age of early symptoms around 7 months but could become symptomatic into adulthood (Leblanc, 2017)
- CT Imaging should be performed emergently in those who present in respiratory distress (Leblanc, 2017)
- Once symptomatic the primary treatment is surgical resection quickly, as recurrent infections further complicate resection (David, 2016)
- Best timing of surgical resection is thought to be between 6 months and 2 years, allowing time for compensatory growth and to avoid malignant transformation (Leblanc, 2017 and David, 2016)
- Post-operative complications include pleural effusions, fistulas, and hemorrhages (David, 2016)
Moral of the Morsel
- Ultrasound isn’t perfect. I know we already know this, but it especially true when you are talking about trying to obtain images on a wiggling fetus somewhere around the size of a banana.
- Sometimes frequent infections aren’t just back-to-back viruses. I know, we love to say it, and its usually true; however, history and physical exam will go a long way in identifying those who may benefit from additional work up.
- Recurrent pneumonias in the same lobe in a young child? Keep congenital pulmonary anomalies on the differential!
- Consider further imaging in children with abnormal CXR findings. CT can be performed outpatient if asymptomatic in those with suspected CPAM, but it is best performed emergently in those with respiratory distress.
References
Dessole F, Virdis G, Andrisani A, Vitagliano A, Cappadona R, Dessole S, Cosmi E, Capobianco G. Fetal Congenital Cystic Adenomatoid Malformation (CCAM): Pathogenesis, Diagnosis, and Clinical Management: A Case Report. Clinical and Experimental Obstetrics & Gynecology. 2019. Dec 46 (6) 999–1002, https://doi.org/10.12891/ceog5086.2019.
Leblanc C, Baron M, Desselas, E, Phan, MH, Rybak A, Thouvenin G, Lauby C, Irtan S. Congential pulmonary airway malformations: state-of-the-art review for pediatrician’s use. Eur J Pediatr. 2017. Dec 176(12): 1559-1571. PMID: 29046943
Mafalda D, Lamas-Pinheiro R, Henriques-Coelho T. Prenatal and Postanatal Management of Congenital Pulmonary Airway Malformation. Neonatology. 2016. Apr 110 (2): 101-15. PMID: 27070354
Mehta AA, Viswanathan N, Vasudevan AK, Paulose, R, Abraham, M. Congential Cystic Adenomatoid Malformation: A Teritriay Care Hospital Experience. J Clin Diagn Res. 2016. Nov: 10 (11): SC01-SC04. PMID: 28050458
Salerno M, Sessa F, Cocimano G, Roccuzzo S, Esposito M, Pomara C. Congenital Cystic Adenomatoid Malformation (CCAM) Type II: A Rare Case of Sudden Infant Death. Children. 2022. Dec: 9 (12): 1830. https://doi.org/10.3390/children9121830. PMID: 36553274

