Kounis Syndrome
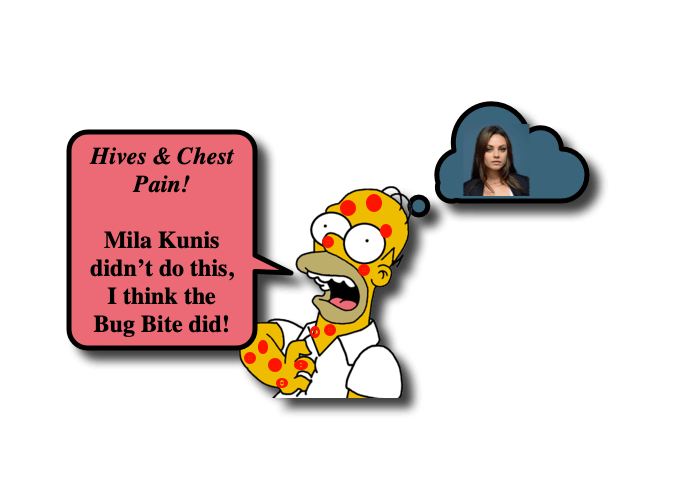
Although it is less common for children to present with cardiac problems than respiratory problems in the ED, every so often there is a little heart that has a big problem. We have previously discussed some cardiac causes of chest pain. Sometimes children can develop cardiac arrhythmias, including catecholaminergic polymorphic ventricular tachycardia, commotio cordis, atrial fibrillation, and short QT syndrome. We have also discussed when children have allergic reactions, they can have a reaction that is relatively minor, like diaper dermatitis, maybe a bit more impressive, like pediatric urticaria, or serious like anaphylaxis. But what happens when the two (allergic reaction and cardiac insult) mix together? Badness, that’s what… and the offspring’s name is Kounis Syndrome. Let’s explore how an allergic reaction can cause a child to essentially have a heart attack.
Kounis Syndrome – Basics
- Also known as “allergic angina” [Kounis 1991]
- First described by Kounis and Zavras in 1991 [Kounis 1991]
- It’s a coronary hypersensitivity reaction
- Usually in 40-70 year olds, but can happen in children [Abdelghany 2017]
- Prevalence 1.1% of allergic inpatient admissions [Giovannini 2020]
- One article defined it as “the concurrence of acute coronary syndromes associated with mast-cell and platelet activation in the setting of allergic or anaphylactic insults” [Abdelghany 2017]
- Histamine and mast cell activation induces coronary artery spasms or acute coronary syndrome, increased intimal thickening, and platelet activation [Kounis 1991, Abdelghany 2017, Giovannini 2020]
- There are H1 and H2 receptors on the 4 heart chambers and the coronary arteries
- Can be provoked by acute allergic reactions to medications, food, environmental factors and other triggers
- Mast cell degranulation releases inflammatory mediators due to an antigen-antibody reaction
- Triggers the complement cascade
- 80% of cases within first hour of exposure
- Inflammatory mediators include: histamine, neutral proteases chymase, tryptase, heparin, cathepsin-D, leukotrienes
- There are 3 subtypes or variants [Abdelghany 2017, Giovannini 2020]
- “Vasopastic allergic angina” – Type 1, most common
- “Allergic myocardial infarction” – Type 2
- “Stent thrombosis with occluding thrombus infiltrated by eosinophils and/or mast cells” – Type 3
- Likely is underdiagnosed
Kounis Syndrome – Presentation and Exam
- Symptoms can include: [Kounis 1991, Abdelghany 2017, Giovannini 2020]
- Chest discomfort (angina pectoris)
- Dyspnea
- Dizziness or faintness
- Nausea, vomiting, abdominal pain
- Urticaria
- Pruritis
- Pallor
- Cold extremities
- Syncope
- Anaphylaxis symptoms- urtcaria, angioedema, itching, wheezing
- Associated with: [Kounis 1991, Abdelghany 2017, Giovannini 2020]
- Hypotension
- Diaphoresis
- Pallor
- Bradycardia, tachycardia
- EKG findings: [Kounis 1991, Abdelghany 2017, Giovannini 2020]
- Suggests myocardial ischemia
- Arrhythmias
- Conduction delays
- Causes or triggers of Kounis syndrome: [Kounis 1991, Abdelghany 2017, Giovannini 2020]
- Most often induced by antibiotics (27.4%), then insect bites (23.4%) [Abdelghany 2017]
- Medication-induced
- Metronidazole [Terlemez 2015]
- Mesalamine [Kounis 2008]
- Diclofenac [Pejcic 2023]
- Anesthesia medications [Capponi 2021]
- Atropine [Castellano Martinez 2018]
- Insect-induced
- Black widow spider bite [Yaman 2015]
- Bee sting [Tripathi 2020, Bodur 2022]
- Wasp sting [Selcuk 2022]
- Scorpion sting [Verma 2021]
- Immunotherapy-induced
- Weekly allergy immunotherapy injection [Mason 2023]
- Contact with substances
- Latex [Rodríguez-González 2019]
Kounis Syndrome- Diagnosis
- Based on clinical symptoms, labs, EKG, echocardiography, and angiography [Abdelghany 2017]
- Can be difficult to recognize and is under reported [Giovannini 2020]
- Recommended labs [Abdelghany 2017]
- Complete blood count (CBC): attention to eosinophils
- Cardiac enzymes (CK, CK-MB) and troponin I or T
- C-reactive protein (CRP, high sensitivity)
- Total and specific immunoglobulin E (IgE)
- Histamine, chymase, tryptase serum levels
- Histamine has short 8 minute half life. Negative level doesn’t rule out Kounis syndrome
- Arachidonic acid products: thromboxane, leukotrienes, prostaglandins
- Tumor necrosis factor (TNF), interferon (INF), interleukin-6 (IL6)
- EKG will show ST-T changes consistent with ischemia, including STEMI, especially in the inferior leads
- T wave changes
- Arrhythmias, and heart block
- QRS or QT prolongation
- Echocardiogram can show regional wall abnormalities in the coronary artery distribution
- Right coronary artery in >50% of cases
- Chest Xray
- Angiography
- Dynamic contrast-enhanced MRI
- Myocardial single-photon emission CT (SPECT)
Kounis Syndrome – Treatment
- Myocardial revascularization along with treatment of allergic reaction [Abdelghany 2017, Giovannini 2020]
- For the allergic reaction
- Corticosteroids – hydrocortisone 1-2 mg/kg/day
- Diphenhydramine – 1-2 mg/kg
- Ranitidine – 1 mg/kg
- Fluid resuscitation to treat shock
- Use epinephrine with caution! May worsen myocardial ischemia, prolong QTc interval, induce coronary vasospasm and arrhythmias
- Use if indicated, but be vigilant for complications.
- Can also consider using methoxamine if patient doesn’t respond to epinephrine
- Caution with beta blockers as they can exacerbate symptoms due to uninhibited alpha
- Morphine, codeine, and meperidine are often used for pain control with chest pain, but use with caution as these can induce further mast cell degranulation [Kounis 2016]
- Acetaminophen can cause hypotension in this setting, especially intravenously [Kounis 2016]
- Fentanyl only causes minimal mast cell activation but is the preferred pain medication [Kounis 2016]
- Vasodilators – calcium channel blockers, nitrates – can be useful to relieve vasospasm
Kounis Syndrome – Complications
- Complete recovery is expected with proper treatment, and complications are rare [Abdelghany 2017, Giovannini 2020]
- Cardiogenic shock (2.3%)
- Cerebrovascular events
- Arrhythmias
- Venous thromboembolisms
- Cardiac arrest (6.3%)
- Death (2.9%-7.0%)
Morel of the Morsel
- Myocardial infarction IS possible in kids! Think of Kounis syndrome when a child has chest pain in the setting of an allergic reaction.
- Simple things can cause complications! Allergic reactions that lead to Kounis syndrome can be triggered by things as “simple” as antibiotics and insect bites.
- Be vigilant with the medications you typically use to treat allergic reactions and pain! They may not be the best first line medications in Kounis Syndrome!
References
- Kounis NG, Zavras GM. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract. 1991;45(2):121-128.
- Abdelghany M, Subedi R, Shah S, Kozman H. Kounis syndrome: A review article on epidemiology, diagnostic findings, management and complications of allergic acute coronary syndrome. Int J Cardiol. 2017;232:1-4. doi:10.1016/j.ijcard.2017.01.124
- Giovannini M, Koniari I, Mori F, et al. Kounis syndrome: a clinical entity penetrating from pediatrics to geriatrics. J Geriatr Cardiol. 2020;17(5):294-299. doi:10.11909/j.issn.1671-5411.2020.05.011
- Giovannini M, Alletto A, Koniari I, et al. Kounis Syndrome: a pediatric perspective. Minerva Pediatr. 2020;72(5):383-392. doi:10.23736/S0026-4946.20.06007-7
- Terlemez S, Eryılmaz U, Tokgöz Y, Uysal P, Coşan A, Bulut Y. Kounis syndrome caused by metronidazole–a case of 14 year-old boy. Int J Cardiol. 2015;179:222-224. doi:10.1016/j.ijcard.2014.11.049
- Kounis GN, Kouni SA, Hahalis G, Kounis NG. Mesalamine hypersensitivity and Kounis syndrome in a pediatric ulcerative colitis patient. World J Gastroenterol. 2008;14(46):7141-7142. doi:10.3748/wjg.14.7141
- Pejcic AV, Milosavljevic MN, Jankovic S, Davidovic G, Folic MM, Folic ND. Kounis Syndrome Associated With the Use of Diclofenac. Tex Heart Inst J. 2023;50(1):e217802. doi:10.14503/THIJ-21-7802
- Capponi G, Giovannini M, Koniari I, et al. Case Report: Perioperative Kounis Syndrome in an Adolescent With Congenital Glaucoma. Front Cardiovasc Med. 2021;8:676188. Published 2021 Sep 10. doi:10.3389/fcvm.2021.676188
- Castellano-Martinez A, Rodriguez-Gonzalez M. Coronary artery spasm due to intravenous atropine infusion in a child: possible Kounis syndrome. Cardiol Young. 2018;28(4):616-618. doi:10.1017/S1047951117002785
- Yaman M, Mete T, Ozer I, Yaman E, Beton O. Reversible Myocarditis and Pericarditis after Black Widow Spider Bite or Kounis Syndrome?. Case Rep Cardiol. 2015;2015:768089. doi:10.1155/2015/768089
- Tripathi S, Kulikowska A, Patel PM, Hassan NE. Acute Myocardial Ischemia Following Bee Sting in an Adolescent Male: A Case Report. Am J Case Rep. 2020;21:e922120. Published 2020 May 29. doi:10.12659/AJCR.922120
- Bodur İ, Yaradılmış RM, Güngör A, Sel K, Tuygun N. A rare pediatric case of Kounis syndrome after bee sting. Acta Clin Belg. 2022;77(4):782-784. doi:10.1080/17843286.2021.1981587
- Selcuk A, Gullu UU. Kounis syndrome after a wasp sting. J Paediatr Child Health. 2022;58(1):173-174. doi:10.1111/jpc.15423
- Mason M, Campbell MD. Kounis syndrome following allergy injection in a paediatric patient. Cardiol Young. 2023;33(2):331-333. doi:10.1017/S1047951122002086
- Verma S, Mathew R, Khan KM, Gouthami V. Allergic myocardial infarction (Kounis syndrome) in a child with scorpion sting. Ann Pediatr Cardiol. 2021;14(3):441-442. doi:10.4103/apc.apc_257_20
- Rodríguez-González M, Castellano-Martínez A. Vasoespasmo coronario en un niño alérgico al látex: síndrome de Kounis [Coronary vasospasm in a child allergic to latex: Kounis syndrome]. Arch Argent Pediatr. 2019;117(5):e514-e518. doi:10.5546/aap.2019.e514
- Kounis, Nicholas G.. “Kounis syndrome: an update on epidemiology, pathogenesis, diagnosis and therapeutic management” Clinical Chemistry and Laboratory Medicine (CCLM), vol. 54, no. 10, 2016, pp. 1545-1559. https://doi.org/10.1515/cclm-2016-0010

