Catecholaminergic Polymorphic VTach
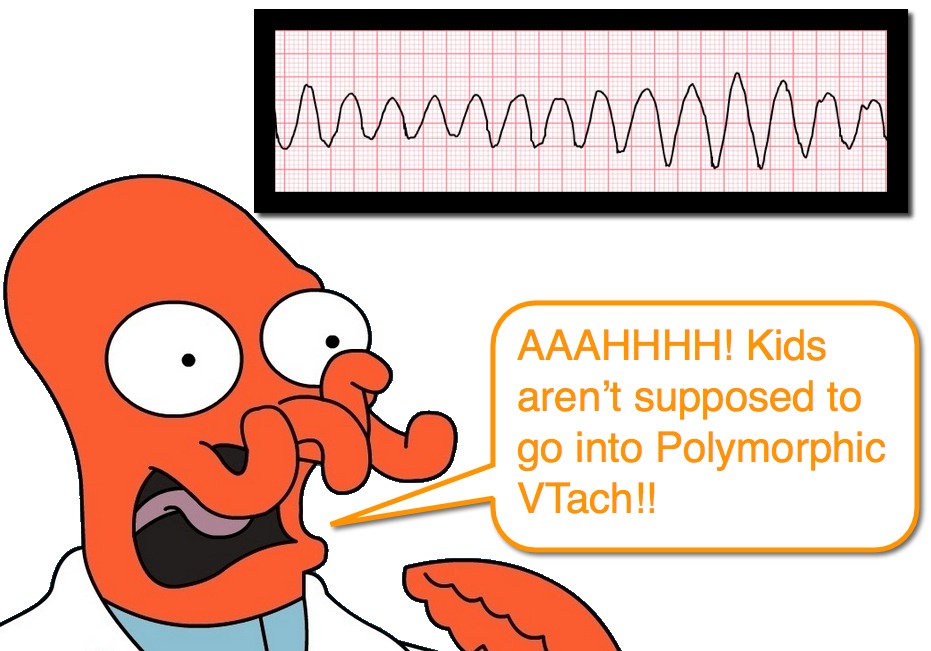
Honestly, one of the best aspects of writing the Ped EM Morsels weekly is that I benefit from learning (or re-learning) something each week. This week is a great example of that phenomenon. We do not often have to care for the pediatric cardiac arrest, but when we do we take comfort in our advanced training and can rely on some of the basic concepts and recommendations (AHA Resuscitation Guidelines). What happens, though, when our advanced life support training steers us in the wrong direction? Let us consider the unusual case of Catecholaminergic Polymorphic Ventricular Tachycardia.
Catecholaminergic Polymorphic VTach: Basics
- Rare, but important cause of syncope or sudden death in kids.
- Mortality as high as 35% by age 30 years when untreated.
- Worse prognosis for those who present earlier in life.
- Malignant arrhythmogenic disorder that is characterized by:
- Structurally normal heart,
- Unlike Hypertrophic Cardiomyopathy.
- Unlike Arrhythmogenic Right Ventricular Dysplasia
- Normal baseline ECG (some may have borderline long QTc),
- Unlike Long QT Syndrome
- Unlike Short QT Syndrome
- Unlike Brugada Syndrome
- Unlike Wold-Parkinson-White Syndrome
- Polymorphic VTach induced by:
- Exercise or
- Emotional Stress or
- Other cause of Increased Catecholamines (ex, illicit substances)
- Structurally normal heart,
- Generally presents between ages of 7 and 9 years.
- Uncommon to present before age 2 years.
Catecholaminergic Polymorphic VTach: Genetics
- Family history of exercise-related syncope, seizure, or sudden death is reported in 30% of cases.
- Caused by gene mutations.
- Likely several genes involved, but two are known (RyR2 and CASQ2)
- Both encode of proteins that regulate intracellular calcium!
- It is recommended that other family members are tested and treated if found to have the genes.
Catecholaminergic Polymorphic VTach: Presentation
- Typically will present with syncope and/or “seizure.”
- Often initially misdiagnosed as either seizure or benign cause of syncope.
- Mean delay in correct diagnosis is ~ 2 years.
- Resting ECG is normal.
- There is progressive ventricular ectopy as the heart rate increases.
- Between 100-120 beats per minute there is increasing complexity.
- First isolated PVCs evolve to bigeminy and then runs of nonsustained VTach.
- Eventually, sustained VTach and Polymorphic VTach are observed.
Catecholaminergic Polymorphic VTach: Daily Therapy
- It is recommended that ALL phenotypically and genotypically diagnosed individuals receive therapy.
- OPTIONS:
- Beta-Blockers
- 1st line
- Nadalol is often used
- Implantable Cardioverter Defibrillator (ICD)
- Used for those who fail medications or for those who present with an aborted cardiac arrest.
- Should be used concurrently with beta-blockers to avoid electrical storm caused by the adrenergic surge from the shocks.
- Flecainide
- Verapamil
- Left Cardiac Sympathetic Denervation
- Beta-Blockers
- Also recommended that they avoid competitive sports or other stimulants.
Catecholaminergic Polymorphic VTach: ACUTE Therapy
- Managing a patient with CPVT who is in VTach can be tricky.
- The most important step is recognizing that the patient has Catecholaminergic Polymorphic VTach.
- Family history is integral!
- Previous history of syncope or seizure can raise suspicion for it as well.
- Standard use of Epinephrine during the resuscitation can be counterproductive.
- IV beta-blockers is considered first choice, similar to VTach storm of other etiologies.
- Given that it is Polymorphic VTach, it would also be reasonable to administer Magnesium, but this would be aimed at possible Prolonged QTc.
Moral of the Morsel
- This represents a significant challenge for us in the Emergency Department. It is rare and can present in a benign fashion (syncope). Even those who are thorough and obtain an ECG may be inappropriately reassured by the normal ECG.
- The patient who has had a SYNCOPAL event deserves consideration for multiple entities (ex, Prolonged QTc, SVT) and should have a screening ECG.
- Ask about family history! You can’t outrun your genes.
- Ask about prior syncopal events that were associated with exciting or stressful situations.
- Don’t always assume wellness just because the patient is young.
References
Leenhardt A1, Denjoy I, Guicheney P. Catecholaminergic polymorphic ventricular tachycardia. Circ Arrhythm Electrophysiol. 2012 Oct;5(5):1044-52. PMID: 23022705. [PubMed] [Read by QxMD]
Pflaumer A1, Davis AM. Guidelines for the diagnosis and management of Catecholaminergic Polymorphic Ventricular Tachycardia. Heart Lung Circ. 2012 Feb;21(2):96-100. PMID: 22119737. [PubMed] [Read by QxMD]
Napolitano C1, Bloise R, Monteforte N, Priori SG. Sudden cardiac death and genetic ion channelopathies: long QT, Brugada, short QT, catecholaminergic polymorphic ventricular tachycardia, and idiopathic ventricular fibrillation. Circulation. 2012 Apr 24;125(16):2027-34. PMID: 22529064. [PubMed] [Read by QxMD]
Heiner JD1, Bullard-Berent JH, Inbar S. Deadly proposal: a case of catecholaminergic polymorphic ventricular tachycardia. Pediatr Emerg Care. 2011 Nov;27(11):1065-8. PMID: 22068070. [PubMed] [Read by QxMD]
van der Werf C1, Zwinderman AH, Wilde AA. Therapeutic approach for patients with catecholaminergic polymorphic ventricular tachycardia: state of the art and future developments. Europace. 2012 Feb;14(2):175-83. PMID: 21893508. [PubMed] [Read by QxMD]


[…] More: Catecholaminergic Polymorphic VTach (Pediatric EM […]