Tibial Tubercle Avulsion Fracture
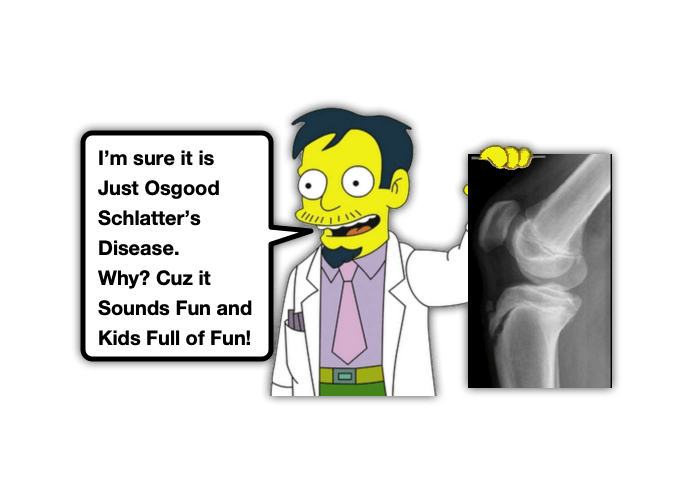
Pediatric x-rays are challenging. Of course, we want children to grow, but those darn growth plates really make interpretation of their films difficult!! We have previously discussed how the surrounding ligaments and tendon are often stronger than the weakest part of the child’s bone necessitating our vigilance when addressing the pediatric extremity complaint (ex, Ankle Pain, Elbow Injury, Supracondylar Fractures). While there are significant injuries that we need to consider, often the real injury is more benign, like Osgood-Schlatter’s Disease. Of course, we cannot assume all anterior knee pain is benign. There may be a patellar sleeve injury or patellar tendon rupture. There is also another specific injury that may mimic Osgood-Schlatter’s Disease, but is more sinister and potentially limb threatening. Let’s take a minute to digest a morsel on this unique injury – the Tibial Tubercle Avulsion Fracture:
Tibial Tubercle Avulsion Fracture: Basics
Who gets these and how?
- Typically adolescent males (10:1 male to female predominance)
- Average age between 9-14 years when children are nearing skeletal maturity
- Seen mostly in athletes who participate in sports with jumping (concentric contraction of quadriceps) and forced knee flexion, but also seen in sports that require explosive use of lower extremities such as track, volleyball, gymnastics etc.
What anatomy should you be aware of?

- 4 stages of ossification of the tibial tubercle: Cartilaginous (8-9 years), Apophyseal (8-14 years), Epiphyseal (10-17 years), and Osseous (15-17 years)
- Most susceptible to injury during apophyseal phase
- Why? The secondary ossification centers are fusing and connecting the proximal aspect of the tibia with the tibial tubercle and the fibrocartilage that is more resistant to tensile forces is slowly replaced with physeal hypertrophic columnar cartilage going from the proximal to distal direction.
- Anterior tibial recurrent artery can be compromised by fractures in this area
Tibial Tubercle Avulsion Fracture: Presentation
- Pain over anterior proximal tibia and tibial tubercle
- History typically involves a known injury with inability to ambulate immediately following
- May have an effusion or hemearthrosis that extends above and below the knee
- Difficulty extending against resistance or gravity depending on severity of injury
- It is important check anterior compartments of lower extremity as injury to anterior tibial recurrent artery can predispose the patient to compartment syndrome
- Patella alta: patellar tendon injuries are seen in 2-15% of tibial tubercle avulsion fractures, ligamentous injuries, meniscal injuries
Tibial Tubercle Avulsion Fracture: Imaging

- Typically an AP and lateral X-rays of the knee will be sufficient, however in subtle cases, bilateral knee X-rays may be helpful for comparison
- The lateral film is the most important as it is the view that classification systems for fracture care are based on
- Though advanced imaging is rarely necessary, it can be helpful if there is concern for intra-articular involvement (ie hemarthrosis)
Tibial Tubercle Avulsion Fracture: Management
- Driven by classification systems that guide whether treatment will be surgical or not.
- Most commonly used is the Ogdon Classification system (a modification of the Watson-Jones criteria). Has undergone many modifications as well to include up to 5 types.
- type I: fracture of the secondary ossification center near the patella tendon insertion
- type II: fracture between the primary and secondary ossification centers
- type III: fracture that traverses the primary and secondary ossification centers
- type IV: fracture through the entire physis
- type V: avulsion of the periosteal sleeve
- The most common type of fracture is a Type-III.
- In general, non-operative treatment is reserved for Type I fractures and type II.
- Type III, IV and V will involve a trip to the OR with Orthopedics for an open reduction.
- Non-operative management is appropriate if extensor mechanism is intact and the avulsed fragment is displaced less than 2 mm or able to be reduced (hyperextension at the knee) to an acceptable degree of displacement.
- Will need about 6 weeks in a long leg cast without weight bearing until cleared by the orthopedic team.
- Involve the orthopedic team early and admit for observation and serial compartment checks if there is concern for developing compartment syndrome.
Moral of the Morsel:
- Growth Plates are Help them Grow to be strong… but are Weak! Always take a pause before you diagnose a “sprain” in a child.
- Anterior knee pain is not always Osgood Schlatter’s. The Athlete is at risk of both Osgood Schlatter’s disease as well as Tibial Tubercle Avulsion Fracture.
References:
Cole, rd et al. “Epidemiology, Diagnosis, and Management of Tibial Tubercle Avulsion Fractures in Adolescents.” JBJS reviews 8.4 (2020): e0186–e0186. Web.
H.P. & Hosalkar, H.S. Tibial tubercle fractures in children with intra-articular involvement: surgical tips for technical ease. J Child Orthop 5, 465–470 (2011). https://doi-org.wake.idm.oclc.org/10.1007/s11832-011-0369-8
Gregory W. Kunis, Joshua A. Berko, Jeffrey C. Shogan, et al. Tibial Tubercle Avulsion Fractures in Adolescents: A Narrative Review & Case Report. Journal of Orthopedics and Orthopedic Surgery. October 26, 2021. (Link)
Howarth, W.R., Gottschalk, H.P. & Hosalkar, H.S. Tibial tubercle fractures in children with intra-articular involvement: surgical tips for technical ease. J Child Orthop 5, 465–470 (2011). https://doi-org.wake.idm.oclc.org/10.1007/s11832-011-0369-8 (classification pictures)
Ogden JA, Tross RB, Murphy MJ (1980) Fractures of the tibial tuberosity in adolescents. J Bone Joint Surg Am 62(2):205–215


How do I share it to my EM Facebook group??