Eyelid Laceration
We all know injuries are a common occurrence in the Ped ED. It has been estimated that ~25% of children seek medical attention each year for an unintentional injury! Now that is a lot of kids (naturally, with a wide range of injury severity)! As is often a point of emphasis with the Ped EM Morsels, we must not allow the frequency of the presentation lead to our complacency.
One of the most common injuries in children is an eyelid laceration. Children just love to lead with their faces when they fall or collide with objects and it is commonly the periorbital area that takes the blow… leading to eyelid lacerations. Certainly, one of our first thoughts is how are we going to keep this squirmy child calm during the repair. While this is an important and noble question, equally important is the question of whether there is any subtle finding in the eyelid laceration that points to more significant injury.
First, Before We Get Ahead of Ourselves
- Many times we want to jump right to the obvious injury, the eyelid laceration, but EyeBall comes before EyeLid in the alphabet and it should also come first during your evaluation!
- You loose style point if you make an excellent repair of the eyelid only to later discover you need to call the Ophthalmologist for the traumatic hyphema.
- Get the Vital Sign of the Eye = Visual Acuity!
- Assess Extraocular Muscles – any evidence of entrapment?
- Check Pupillary Function (any evidence of glaucoma? any afferent pupillary defect?)
- Assess for globe rupture – yes, even with what appears to be a minor eyelid laceration.
- Any asymmetry of the pupil?
- Seidel’s Sign?
- Here is where a portable slit-lamp comes in handy (especially with kids who will be more reluctant to sit in the scary looking slit-lamp machine – I’m scared to sit there too!).
- Look for an anterior chamber that is Deep (the distance from the cornea to the iris).
- Check for hyphema
- Small ones can be missed without magnification – again, use portable slit lamp.
- Large ones can be missed as it occupies the entire pupil – again, check a visual acuity. Also, having the patient sit upright for awhile can help.
- Check for traumatic iritis
- Hmm… that requires a portable slit-lamp also.
- Check for Corneal Abrasions or retained Foreign Bodies (also done better with a portable slit-lamp than Wood’s Lamp)
Now, onto the Eyelid Laceration
-
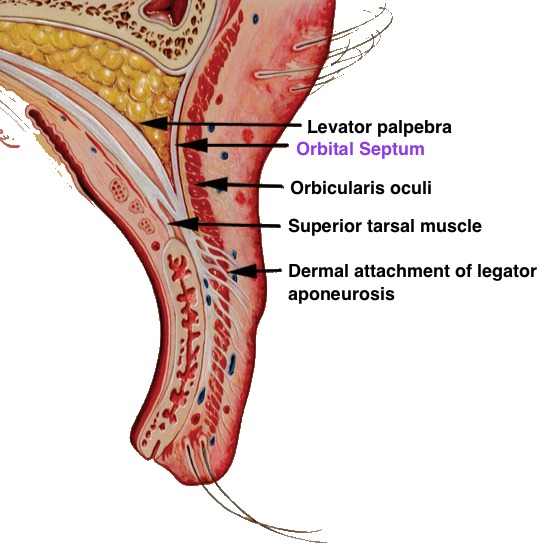
Anatomy is Critical
The eyelid crease is the point where the levator muscle interdigitate with the orbicularis muscle and insert into the skin.
- The orbital septum is the thin membrane that separates the orbit from the outside world. It isn’t that deep. The upper eyelid skin is the thinnest in the body!
- Behind the orbital septum in the upper eyelid there are two fat pads.
- In the lower eyelid, there are three fat pads.
- The most medial aspect of the upper and lower eyelid margin contains a lacrimal punctum.
-
Subtle Signs of More Significant Injury with an Eyelid Laceration
- Exposed Fat
- Fat is on the other side of the orbital septum… if you see, then the injury has penetrated the orbit.
- The globe, extraocular muscles, and optic nerve are at risk of being injured.
- Risk of retained orbital foreign bodies.
- Risk of orbital hematoma and infection.
- It is difficult to asses the true depth of this injury. CT of the orbits will be helpful
- Ptosis
- Indicating injury to the levator mechanism
- Exposed Fat
- Fluorescein dye that has not disappeared.
- Indicates potential lacrimal system injury.
- This should also be considered for any injury that involves the area medial / nasal to the puncta.
Karesh JW. Chapter 75: The Evaluation and Management of Eyelid Trauma in Duane’s Ophthalmology on CD-ROM, 2006 Edition. http://www.oculist.net/downaton502/prof/ebook/duanes/index.html


[…] care is a common issue in the ED. Certainly, not all wounds are created equal. We have discussed eyelid lacerations and tongue lacerations. We have also discussed my favorite wound closure technique: tissue […]
[…] Eyelid Laceration -Nice Review of a deceptively difficult diagonsis and management problem. […]