May-Thurner Syndrome in Children
In the Pediatric Emergency Department, sometimes compression is a helpful thing (Chest Compressions, Epistaxis), and sometimes compression isn’t so good (Thoracic Outlet Syndrome, Tourniquet Syndrome, Cardiac Tamponade, Compartment Syndrome). A recent discussion with some colleagues about some interesting cases they have seen prompted me to remember this compression syndrome that I have seen a handful of times – May-Thurner Syndrome. Don’t PRESS me for too much information, but I’ll see what I can SQUEEZE into a few short lines here:
May-Thurner Syndrome: Basics
[Mangla, Mako, Poyyamoli, Fereydooni, Harbin]
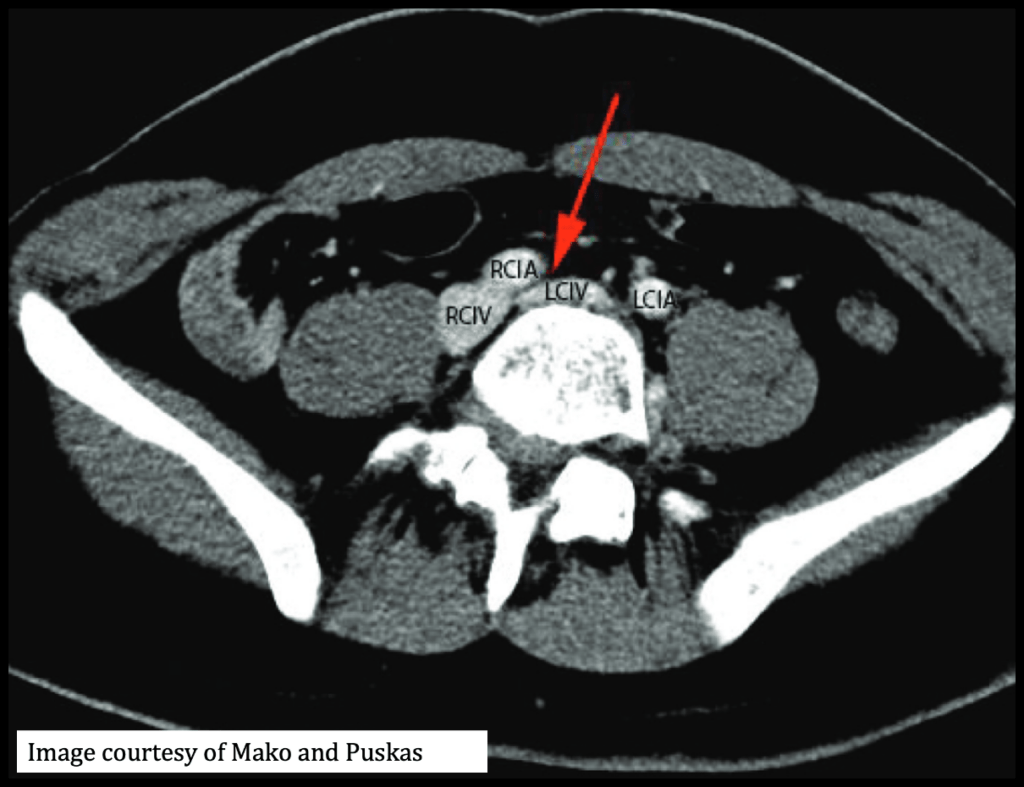
- Compression of the left common iliac vein (LCIV) between the right common iliac artery (RCIA) and the vertebrae, leading to thrombosis.
- There have also been reports of this being RIGHT sided as well.
- Also known as “Cockett Syndrome” or “Iliac Vein Compression Syndrome”
- Occurs after the origination from the aorta and before the iliofemoral junction
- Chronic endothelial irritation from pulsation of the overlying artery is theorized to cause “venous spurs” leading to fibrous band and clot formation.
- It causes 2-5% of clinical DVTs, maybe even up to 49% of left sided DVTs.
- Cadaveric studies show a higher prevalence (14-32%)
- Female to male incidence is 2:1
- May be asymptomatic with non-critical obstruction until a trigger, like pregnancy or surgery, causes worsening DVT.
- Most common in 2nd and 3rd decades of life.
May-Thurner Syndrome: Presentation and Exam
- Unilateral swelling or leg pain [Mangla, Poyyamoli]
- Sign/symptoms may be subtle: [Mangla, Poyyamoli]
- Left leg tightness, mild swelling,
- Telangiectasias, venous ulcers [Mangla, Poyyamoli]
- Signs of chronic venous insufficiency: [Mangla, Poyyamoli]
- Hyperpigmentation, lipodermatosclerosis, and recurrent skin ulcers
- Three stages [Mangla, Mako]
- Stage 1- compression without structural changes of vein. Asymptompatic.
- Stage 2- Venous spur or fibrous connection restrict flow and increase risk for DVT and edema
- Stage 3- Venous obstruction causing DVT, swelling, and varicose veins
May-Thurner Syndrome: Diagnosis
[Mangla, Mako, Poyyamoli, Fereydooni ]
- Ultrasound with Doppler
- Most common technique used in the ED. First line evaluation.
- Great at diagnosing DVTs
- BUT, technically challenging to find iliac vein compression with Doppler alone
- Not the ideal study.
- CT Venography
- 95% sensitivity and specificity to diagnose iliac vein compression
- Can find other compression causes- hematoma, tumor, lympadenopathy
- Can’t asses volume status, may overestimate degrees of compression in a dehydrated patient
- Magnetic Resonance Venography
- Single snapshot may not be enough to diagnose due to variable LCIV compression over time
- Cost-prohibitive for some
- Venography with intravascular ultrasound (IVUS)
- Gold standard to date
- Is invasive and now reserved for those going for endovascular treatment
- Intravascular ultrasound (IVUS)
- Gaining popularity and use
- Real time evaluation of the vessel lumen
- Can show chronicity of thrombus, helps with management decisions
- Can localize guidewires during recanalizations
- No contrast needed! Less contrast-related nephropathy and allergies!
- Air Plethysmography (APG) [Mako]
- Non-invasive method to quantify venous obstruction
- Outflow fraction calculation
May-Thurner Syndrome: Treatment
- Acute thrombosis- catheter directed thrombolysis with endovascular stent placement [Mangla, Mako, Poyyamoli, Fereydooni ]
- Vascular angioplasty isn’t good enough
- Surgical thrombectomy is falling out of favor
- Reserved for patients who fail endovascular methods
- Bypass is rare but is an option. [Mangla]
- Anticoagulation with low molecular weight heparin, fondaparinux, or warfarin [Mangla]
- Factor Xa inhibitors have been approved for use, but lack data for iliofemoral thrombosis.
- Anticoagulation alone is not enough, though. The CaVenT trial and subgroup analysis of ATTRACT trial concluded that anticoagulation after catheter-directed thrombolysis was superior to anticoagulation alone. [Mangla, Poyyamoli]
- Duration of anticoagulation is controversial and debated [Mako]
May-Thurner Syndrome: Complications
- Post-thrombotic syndrome– wear compression stockings!
- Pulmonary embolism
- Bleeding risks with anticoagulation medications
- Rare: phlegmasia cerulea dolens– life threatening acute DVT complication with extreme swelling of the extremity with pain, cyanosis, and potentially arterial ischemia which leads to gangrene and need for amputation. [Mangla, Chaochankit]
Moral of the Morsel
- For unilateral leg pain and swelling, you may need to look a little deeper to find your answer. The signs and symptoms may be subtle.
- Venography with intravascular ultrasound is the gold standard for diagnosis, but CT venography has benefits.
- Catheter directed thrombolysis, endovascular stent placement, and anticoagulation is the treatment of choice.
- May-Thurner syndrome may be more common than you realize! Stay vigilant and consider LCIV compression!
References
- Mangla A, Hamad H. May-Thurner Syndrome. [Updated 2021 Oct 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554377/
- Mako K, Puskas A. May-Thurner syndrome – Are we aware enough?. Vasa. 2019;48(5):381-388. doi:10.1024/0301-1526/a000775.
- Poyyamoli S, Mehta P, Cherian M, Anand RR, Patil SB, Kalva S, Salazar G. May-Thurner syndrome. Cardiovascular Diagnosis and Therapy. 2021;11(5):1104-1111. doi:10.21037/cdt.2020.03.07.
- Fereydooni A, Stern JR. Contemporary treatment of May-Thurner Syndrome. J Cardiovasc Surg 2021;62:447-55. DOI: 10.23736/S0021-9509.21.11889-0
- Harbin MM, Lutsey PL. May‐Thurner syndrome: History of understanding and need for defining population prevalence. Journal of Thrombosis and Haemostasis. 2020;18(3):534-542. doi:10.1111/jth.14707.
- Chaochankit W, Akaraborworn O. Phlegmasia Cerulea Dolens with Compartment Syndrome. Ann Vasc Dis. 2018;11(3):355-357. doi:10.3400/avd.cr.18-00030

