Transillumination for and Aspiration of Pneumothorax in Neonates
We mentioned in last week’s Morsel that for neonates not responding to resuscitative efforts, that you can transilluminate the chest to determine if there is a pneumothorax present. Let’s finish that discussion:
Neonates are prone to developing a pneumothorax.
- Lack of surfactant makes premature lungs stiff and fragile.
- The child who requires bagged respirations is at risk of having iatrogenic ptx (why we need to pay attention to the pressure that we are using)
- The resuscitative efforts can be thwarted by an undiagnosed pneumothorax
- The very compliant chest wall allows for increased intrathoracic pressures to be more directly related to the right atrium and, thus, leading to decreased Preload and cardiac output.
- In addition, neonates will become bradycardic merely from hypoxia.
Certainly the preferred diagnostic test would be a Chest X-Ray, but… there often isn’t time.
- In a pinch, you can use Tranillumination of the chest to help with your diagnosis
- Place light source (otoscope, transilluminator) on infant’s chest. Ensure it isn’t hot.
- A normal chest will have a small glowing “Halo” around the light source. Usually it extends less than 1 cm from the light source and is symmetric.
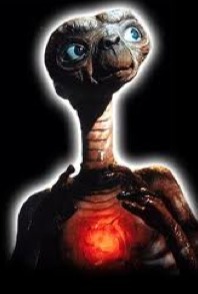
- If the chest “lights up like a jack-o-lantern or ET’s chest” (large area of redness that is often asymmetric), then ptx should be HIGH on your DDx list.
- You should compare to the other side if you are unsure.
So, you’ve just diagnosed a pneumothorax in a neonate, now what do you do? ANSWER = Aspirate
- Aspiration of pneumothorax (Click here to see video)
- Indication
- Traditionally used to relieve tension pneumothorax.
- In small children and neonates, may be the definitive procedure for simple pneumothorax.
- More compliant chest wall and elastic tissues in kids may allow for the hole to spontaneously seal after the procedure so that you don’t have to follow it up with a traditional chest tube.
- If the ptx re-accumulates after aspiration, then a thoracostomy tube will need to be placed (but give the kid a chance first).
- Contraindication
- No strict contraindications
- Equipment
- Angiocath or butterfly needle (for neonates)
- Large syringe (>20mL)
- 3-way stop-cock (to keep system closed)
- Procedure
- Locate 2nd or 3rd intercostal space at the midclavicular line
- Prep skin with antiseptic and provide analgesic/anesthetic.
- Advance needle perpendicularly over superior border of rib while aspirating. Having saline in syringe will allow you to detect when you’ve entered the ptx.
- When bubbles are present or you have free movement of the syringe plunger, evacuate the pneumothorax.
- A 3-way stopcock can be placed between syringe and butterfly needle, which will allow for controlled evacuation of pneumothorax.
- Complications
- Injury to neurovascular bundle
- Injury to thoracic organs
- Indication
Baldwin, S. and T.E. Terndrup, Thoracostomy and Related Procedures, in Textbook of Pediatric Emergency Procedures, 2nd Edition, C. King and F.M. Henretig, Editors. 2008, Lippincott Williams & Wilkins. p. 355-390.