Typhlitis
We all care for many children who present with fever, nausea, and vomiting. Naturally, one of our first goals is to consider severe and life-threatening conditions and, fortunately, many times these are apparent on clinical exam. Unfortunately, certain patient populations, especially the pediatric oncology patient, may present with nonspecific symptoms and have a nonspecific exam but end up having a very specific and significant condition: Typhlitis.
Typhlitis Basics:
- Necrotizing inflammation of the colon, cecum, and / or terminal part of the ileum.
- Also known as “Neutropenic colitis” (although the patient does not have to be strictly neutropenic).
- Associated with:
- Underlying Malignancy
- Intensive Chemotherapy
- Severe Neutropenia
- Incidence = 0.35% to 10% of children with malignancies (depending on the study).
- In recent years, with the use of more intensive chemotherapy regimens, there has been an increase in incidence of typhlitis.
Dangers of Typhlitis:
- May progress to full thickens necrosis and Bowel Perforation! {that’s suboptimal}
- May lead to intestinal hemorrhage. {also subpar}
- The injured intestine may act as an entry point for bacteria to transmigrate into bloodstream and lead to Sepsis. {nuff said}
- Mortality rates of Typhlitis range from 2.2% to 48%.
Causes of Typhlitis:
- Strictly speaking, it is not fully known.
- Suspected culprits:
- Drug-induced GI ulcerations
- Neutropenia leading to invasive bacteria related mucosa damage
- Sepsis-induced hypotension leading to bowel ischemia
- Combination of all…
Typhlitis Presentation:
- Initially, the presenting symptoms can be very nonspecific:
- Crampy Abdominal Pain
- Diarrhea
- Nausea
- Vomiting
- Right Lower Quadrant Pain
- Fever
- The “Classic Triad” — unfortunately, “Classic” doesn’t mean Definitive.
- Abdominal Pain -absent in 9% in one study
- Fever – absent in 16% in one study
- Neutropenia – absent in 12% in one study
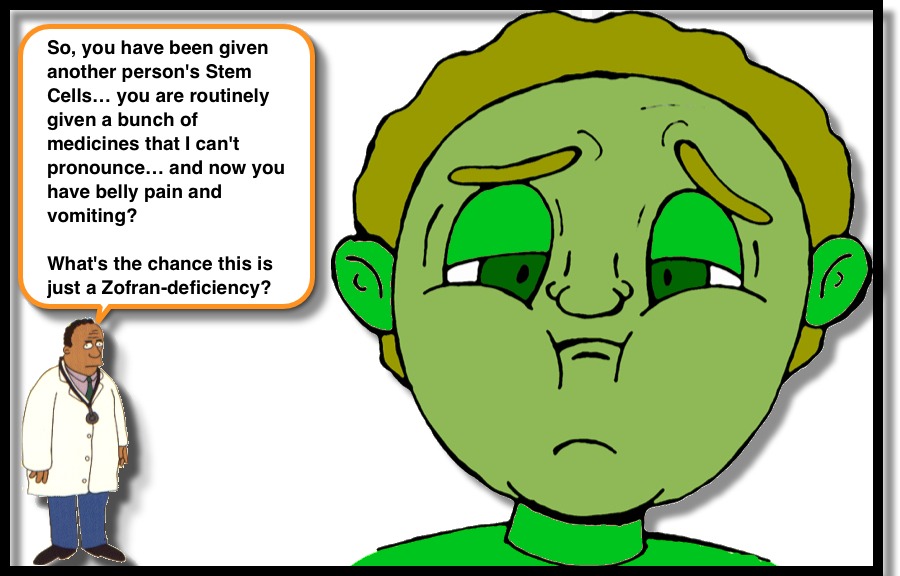
Typhlitis Increased Risk Factors:
- Having received chemotherapy in previous 2 weeks.
- Pt with mucositis on exam.
- S/P Stem Cell Transplantation.
- Certain drug regimens confer greater risk (but I can’t pronounce them, so I’d recommend discussing with the pt’s oncologist).
Imaging for Typhlitis:
- Ideal imaging modality is still debated… and likely dependent upon your institutional resources.
- Abdominal X-Ray
- May show small bowel obstruction
- May show fluid-filled cecum
- More useful to look for Free-air and Air-fluid levels.
- Abdominal CT
- Pro: can help differentiate other abdominal pathology.
- Con: Radiation, Bowel Wall thickness does not correlate with severity of typhlitis.
- Abdominal U/S
- Pro: no Radiation. Pt’s tolerate well. The degree of Bowel Wall Thickening has been correlated with severity of disease.
- Con: Operator dependent (so need good institutional experience). Need to evaluate the length of the colon… not just RLQ.
Therapy for Typhlitis:
- Generally, conservative management is successful, when detected early in the course of the condition.
- NPO
- IVF
- Broad Spectrum Antibiotics (ex:…)
- Ceftazidime
- Meropenem
- Pip/Tazo
- Metronidazole
- Surgical intervention should be used for bowel perforation, persistent GIB, or clinical deterioration despite optimal medical management.
Altinel E, et al. Typhlitis in Acute Childhood Leukemia. Med Princ Pract 2012; 21:36-39.
Moran H, et al. Risk Factors for Typhlitis in Pediatric Patients with Cancer. J Pediatr Hematol Oncol 2009;31:630-634.
McCarville MB, et al. Typhlitis in Childhood Cancer. Cancer 2005;104(2):380-387.


Thank you Dr Sean ,I have a patient who is 4years old with typhlitis after chemotherapy of ALL, he has all the systoms and signs mentioned above . Including difficult in breathing because of ascities.Thanks for the management info.
My grandson was diagnosed with typhlitis. You didn’t mention high heart rate and difficulty breathing…he’s 4 and his heartrate is finally lowering to the 130’s after 5 days…and he’s still receiving oxygen. Is this consistent with typhlitis or could something else be going on?
Baker Family,
I am sorry to hear that your grandson is ill. I cannot speak specifically about individual’s medical care… but can say that high heart rates (elevated pulse) is something that is seen in many conditions. Often it is related to the child (or adult for that matter) trying to compensate for the illness that she/he is suffering with.
Hope all improves,
sean
[…] Typhlitis (neutropenic enterocolitis) – […]