Peritonsillar Abscess
Peritonsillar Abscess: Basics
- Peritonsillar abscess is the most common deep space head and neck infection.
- In children, it accounts for 49% of head and neck infections. [Ungkanont, 1995]
- Retrophayrngeal abscess account for 22%. [Ungkanont, 1995]
- Collection of pus located between the tonsillar capsule, the superior constrictor and the palatopharyngeus muscle. [Schraff, 2001]
- Complications:
- Spread to other contiguous structures and into the parapharyngeal space and deeper.
- Acute enlargement of the tonsillar pillars causing airway constriction!
- Spontaneous rupture of tonsil and acute aspiration of purulent material. (yuk)
Peritonsillar Abscess: Diagnostic Challenge
- Peritonsillar Abscess should be a clinical diagnosis.
- The issue is when your clinical exam is limited!
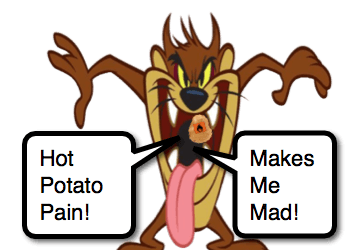
- Some children will not be the most cooperative with the exam.
- Trimus (30-60% of the time) may actually prevent their cooperation. [Schraff, 2001; Ungkanont, 1995]
- Small mouth opening can also obscure your view. [Brodsky, 1988]
- May need to enhance your exam!
- Positioning
- Have child sit on parent’s lap, facing parent, with legs extended around parent’s waist.
- Have child lay backwards onto parent’s legs, ideally so that head extends slightly over the parent’s knees.
- This often leads to some “disorientation” and makes the mouth easier to open.
- Tools
- Ensure good lighting with headlamp (super cool looking too).
- Tongue displacement and good lighting with Magill Laryngoscope (See ALIEM Tricks of Trade)
- Positioning
- Often leads to potential over utilization of CT scans, especially in younger children. [Baker, 2012]
- May require sedated exam in the OR or ED to more accurately make diagnosis. [Schraff, 2001]
- Some children will not be the most cooperative with the exam.
Peritonsillar Abscess: Imaging
- Ideally the image you need is made with your eyeballs, but… if you need see better:
- Certainly CT is very sensitive [Scott, 1999], but comes with other issues.
- CT is close to 100% sensitive.
- Most useful if you are concerned for deeper space infection, like Retropharyngeal Abscess.
- Ultrasound
- Intra-oral Ultrasound (using endocavitary probe)
- Has been shown to be very specific. [Scott, 1999]
- Can be somewhat intimidating for children.
- Trans-cervical Ultrasound (using linear, high frequency probe)
- Tolerated well and is less intimidating (as there is no large probe being projected into the kid’s painful mouth).
- Uses the submandibular and midline approaches. [See Bandarkar, 2015 for nice description]
- Found to be helpful in determining who will not need surgical intervention. [Fordham, 2015]
- Intra-oral Ultrasound (using endocavitary probe)
Peritonsillar Abscess: Management
- Analgesia (please don’t be cruel).
- Optimize hydration status.
- Antibiotics
- Coverage for Streptococcus species is necessary.
- Don’t forget about Fusobacterium!
- Often polymicrobial infections are present.
- Some can even be treated with antibiotics alone. [Nguyen, 2015; Hsiao, 2011]
- Drainage of Abscess
- Needle Aspiration
- Incision and Drainage
- There has been a trend favoring Incision and Drainage over Tonsillectomy. [Qureshi, 2015]
- Quinsy Tonsillectomy
- Tonsillectomy during acute infection.
- Delayed / Interval Tonsillectomy
- Tonsillectomy after resolution of infection.
- Often reported to have less complications, but not necessarily true. [Simon, 2013]
Moral of the Morsel
- Peritonsillar Abscess is common so be familiar with its management.
- The diagnosis is primarily clinical, but the clinical exam can be challenging, so know how to augment your exam.
- If uncertain, start with ultrasound, preferentially starting with trans-cervical images!
- Realize that there are options for management that even include a trial of antibiotic only and reassessment (although I wouldn’t send that one home).
- In older, cooperative patients, it is completely reasonable to manage as you would an adult with Needle Aspiration in the ED.
References
Qureshi H1, Ference E2, Novis S3, Pritchett CV4, Smith SS5, Schroeder JW4. Trends in the management of pediatric peritonsillar abscess infections in the U.S., 2000-2009. Int J Pediatr Otorhinolaryngol. 2015 Apr;79(4):527-31. PMID: 25708703. [PubMed] [Read by QxMD]
Kim DK1,2, Lee JW1, Na YS1, Kim MJ1, Lee JH1,2, Park CH1,2. Clinical factor for successful nonsurgical treatment of pediatric peritonsillar abscess. Laryngoscope. 2015 Nov;125(11):2608-11. PMID: 26152910. [PubMed] [Read by QxMD]
Nguyen T1, Haberland CA1, Hernandez-Boussard T2. Pediatric Patient and Hospital Characteristics Associated With Treatment of Peritonsillar Abscess and Peritonsillar Cellulitis. Clin Pediatr (Phila). 2015 Nov;54(13):1240-6. PMID: 25589309. [PubMed] [Read by QxMD]
Bandarkar AN1, Adeyiga AO2, Fordham MT3, Preciado D4, Reilly BK4. Tonsil ultrasound: technical approach and spectrum of pediatric peritonsillar infections. Pediatr Radiol. 2015 Dec 5. PMID: 26637999. [PubMed] [Read by QxMD]
Fordham MT1, Rock AN2, Bandarkar A3, Preciado D1, Levy M1, Cohen J4, Safdar N3, Reilly BK. Transcervical ultrasonography in the diagnosis of pediatric peritonsillar abscess. Laryngoscope. 2015 Dec;125(12):2799-804. PMID: 25945805. [PubMed] [Read by QxMD]
Simon LM1, Matijasec JW, Perry AP, Kakade A, Walvekar RR, Kluka EA. Pediatric peritonsillar abscess: Quinsy ie versus interval tonsillectomy. Int J Pediatr Otorhinolaryngol. 2013 Aug;77(8):1355-8. PMID: 23810548. [PubMed] [Read by QxMD]
Hsiao HJ1, Huang YC, Hsia SH, Wu CT, Lin JJ. Clinical features of peritonsillar abscess in children. Pediatr Neonatol. 2012 Dec;53(6):366-70. PMID: 23276441. [PubMed] [Read by QxMD]
Baldassari C1, Shah RK. Pediatric peritonsillar abscess: an overview. Infect Disord Drug Targets. 2012 Aug;12(4):277-80. PMID: 22338588. [PubMed] [Read by QxMD]
Baker KA1, Stuart J, Sykes KJ, Sinclair KA, Wei JL. Use of computed tomography in the emergency department for the diagnosis of pediatric peritonsillar abscess. Pediatr Emerg Care. 2012 Oct;28(10):962-5. PMID: 23023458. [PubMed] [Read by QxMD]
Schraff S1, McGinn JD, Derkay CS. Peritonsillar abscess in children: a 10-year review of diagnosis and management. Int J Pediatr Otorhinolaryngol. 2001 Mar;57(3):213-8. PMID: 11223453. [PubMed] [Read by QxMD]
Blotter JW1, Yin L, Glynn M, Wiet GJ. Otolaryngology consultation for peritonsillar abscess in the pediatric population. Laryngoscope. 2000 Oct;110(10 Pt 1):1698-701. PMID: 11037828. [PubMed] [Read by QxMD]
Scott PM1, Loftus WK, Kew J, Ahuja A, Yue V, van Hasselt CA. Diagnosis of peritonsillar infections: a prospective study of ultrasound, computerized tomography and clinical diagnosis. J Laryngol Otol. 1999 Mar;113(3):229-32. PMID: 10435129. [PubMed] [Read by QxMD]
Ungkanont K1, Yellon RF, Weissman JL, Casselbrant ML, González-Valdepeña H, Bluestone CD. Head and neck space infections in infants and children. Otolaryngol Head Neck Surg. 1995 Mar;112(3):375-82. PMID: 7870436. [PubMed] [Read by QxMD]
Brodsky L1, Sobie SR, Korwin D, Stanievich JF. A clinical prospective study of peritonsillar abscess in children. Laryngoscope. 1988 Jul;98(7):780-3. PMID: 3164436. [PubMed] [Read by QxMD]


[…] several potential causes of the neck pain previously (ex, Torticollis, Strep Pharyngitis, Peritonsillar Abscess, Retropharyngeal Abscess, Lymphadenopathy, Lemierre’s Syndrome), but let us take a minute to […]