Testicular Torsion
Torsion is the most significant condition on the DDx of patient with scrotal pain.
Prompt diagnosis is imperative:
- The success rate of saving the testicle decreases after 6-8 hours.
- At 12 hours, is the success rate is near 0% (BUT IT IS NOT Zero… never give up!!).
Epidemiology
- Has 2 peaks of incidence: one peak during 1st year of life and another from 12-18 yrs.
- 50% of patients diagnosed with torsion have had a prior episode of intermittent torsion that had spontaneous resolution.
Exam
- The loss of the cremasteric reflex is commonly described with testicular torsion.
- However, the presence of a cremasteric reflex does not rule-out the diagnosis.
- Numerous studies have demonstrated this.
- In these studies, 8-40% of patients with testicular torsion (some even with severe necrosis) had normal cremasteric reflexes. 1-7
Diagnosis
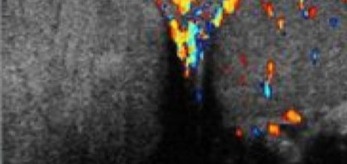
- Color Doppler U/S is the 1st line imagining modality; however, when torsion is considered, time should not be devoted to studies that may prolong the time to surgery… so call your urologist.
- U/S has been found to be useful at depicting whether there is arterial or venous compromise, yet it must still be remembered that it has a sensitivity of only 86-89%. So it isn’t perfect. Don’t ignore your clinical exam and instinct. 8-9
- If an ultrasound is equivocal, radionuclide scans may help reduce false negatives.
1. Van Glabeke E, Khairouni A, Larroquet M, Audry G, Gruner M. Acute scrotal pain in children: results of 543 surgical explorations. Pediatr Surg Int. 1999 Jul;15(5-6):353-7.
2. Murphy FL, Fletcher L, Pease P. Early scrotal exploration in all cases is the investigation and intervention of choice in the acute paediatric scrotum. Pediatr Surg Int. 2006 May;22(5):413-6. Epub 2006 Apr 7.
3. Paul EM, Alvayay C, Palmer LS. How useful is the cremasteric reflex in diagnosing testicular torsion? Journal of the American College of Surgeons. 2004 Sept 199(3):101. Supplement.
4. Ciftci AO, Senocak ME, Tanyel FC, Büyükpamukçu N. Clinical predictors for differential diagnosis of acute scrotum. Eur J Pediatr Surg. 2004 Oct;14(5):333-8.
5. Eaton SH, Cendron MA, Estrada CR, Bauer SB, Borer JG, Cilento BG, Diamond DA, Retik AB, Peters CA. Intermittent testicular torsion: diagnostic features and management outcomes. J Urol. 2005 Oct;174(4 Pt 2):1532-5; discussion 1535.
6. Karmazyn B, Steinberg R, Kornreich L, Freud E, Grozovski S, Schwarz M, Ziv N, Livne P. Clinical and sonographic criteria of acute scrotum in children: a retrospective study of 172 boys. Pediatr Radiol. 2005 Mar;35(3):302-10. Epub 2004 Oct 16.
7. Nelson, C.P., J.F. Williams, and D.A. Bloom, The cremasteric reflex: a useful but imperfect sign in testicular torsion. J Pediatr Surg, 2003. 38(8): p. 1248-9.
8. Kravchick, S., et al., Color Doppler sonography: its real role in the evaluation of children with highly suspected testicular torsion. Eur Radiol, 2001. 11(6): p. 1000-5.
9. Baker, L.A., D. Sigman, R. Mathews, J. Benson, S.G. Docimo, An analysis of clinical outcomes using color Doppler testicular ultrasound for testicular torsion. Pediatrics, 2000 Mar; Col 105, Num 3, pp. 604-607.


[…] Testicular Torsion […]
[…] appropriately. We have already discussed the most feared cause of acute scrotal pain – Testicular Torsion. While there are many other causes of inguinal and scrotal pain (ex, varicocele, inguinal hernia), […]