Epididymitis in Children
Acute Scrotal Pain
- Acute scrotal pain is not uncommon in the Peds ED.
- We have previously discussed some conditions that are related to scrotal pain:
- The most common concerns, however, are:
- Testicular Torsion
- Torsion of the Appendix Testis
- Testicular Tumor
- Acute Epididymitis
Acute Epididymitis in Children
- Epididymitis is not rare in children.
- Older literature described it as a rare condition, but newer research shows greater frequency of disease than previously known. [Nistal, 2016; Redshaw, 2014]
- Majority of cases occur in prepubertal / early adolescent boys (11-14 years). [Redshaw, 2014; Santillanes, 2011]
- Comprises up to 35-65% of all acute scrotal pain cases. [Nistal, 2016]
- Epididymitis is often considered to be due to an infection.
- Older males often have reflux of urine due to prostatic hypertrophy.
- Young males (<35 years) often have an associated sexually transmitted disease.
- What about the children who are not sexually active?
- In young children, the INCIDENCE of infection is LOW. [Nistal, 2016; Santillanes, 2011]
- Of ~1,500 patients with acute epididymitis, only ~15% had positive urine cultures. [Cristoforo, 2016]
- Unfortunately, >85% still received antibiotics. [Cristoforo, 2016; Santillanes, 2011]
- In the end, the majority are classified as idiopathic. [Redshaw, 2014; Min Joo, 2013]
- True etiology is still not fully understood.
- May be due to:
- Inflammation from adjacent torsion of appendix of testis
- Reflux of sterile urine
- Viral illness (ex, Mumps, Coxsackie B, influenza, EBV)
- Anatomic abnormalities (likely in younger patients)
- Trauma
- Epididymitis is usually a unilateral process. [Nistal, 2016]
- The right side is affected more often.
- Hydrocele is usually observed along with local symptoms of inflammation.
Epididymitis: Evaluation/Management
- 1st, don’t overlook the potential for torsion as the etiology!
- Distinguishing epididymitis from testicular torsion clinically can be difficult. [Redshaw, 2014]
- Have low threshold for obtaining Ultrasound.
- If history, exam, and U/S are consistent with epididymitis, consider the age:
- Young boys who are not sexually active
- Low risk for infectious etiology. [Cristoforo, 2016; Santillanes, 2011]
- May wish to treat based on abnormal urinalysis.
- Could also wait until Urine Culture results, as rates of true infections are slow low. [Cristoforo, 2016; Santillanes, 2011]
- Treat with NSAIDs, scrotal support, and rest
- Low risk for infectious etiology. [Cristoforo, 2016; Santillanes, 2011]
- Sexually active boys
- At risk for STDs!
- Consider testing and starting empiric therapy.
- Also can use NSAIDs, scrotal support, and rest (and AVOIDING SEX!).
- Young boys who are not sexually active
Moral of the Morsel
- Don’t overlook torsion! Think of epididymitis as the potential cause of acute scrotal pain in young boys, but check that ultrasound!
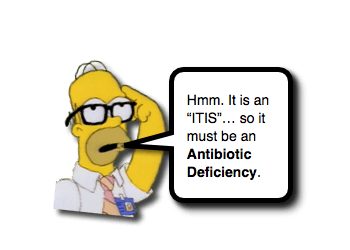
- Just because it has “-itis” at the end of the word, does not mean it is an antibiotic deficiency!
- There is an abundance of antibiotics given to boys with epididymitis who have a low risk for infection. Don’t add to the problem. (see C. Difficile)
- Check a Urine Culture (maybe even resist the urge to react to a urinalysis) and educate the family.
References
Cristoforo TA1. Evaluating the Necessity of Antibiotics in the Treatment of Acute Epididymitis in Pediatric Patients: A Literature Review of Retrospective Studies and Data Analysis. Pediatr Emerg Care. 2017 Jan 17. PMID: 28099292. [PubMed] [Read by QxMD]
Nistal M1, Paniagua R2, González-Peramato P1, Reyes-Múgica M3. Perspective in Pediatric Pathology, Chapter 24. Testicular Inflammatory Processes in Pediatric Patients. Pediatr Dev Pathol. 2016 Nov/Dec;19(6):460-470. PMID: 27575254. [PubMed] [Read by QxMD]
Redshaw JD1, Tran TL2, Wallis MC3, deVries CR4. Epididymitis: a 21-year retrospective review of presentations to an outpatient urology clinic. J Urol. 2014 Oct;192(4):1203-7. PMID: 24735936. [PubMed] [Read by QxMD]
Joo JM1, Yang SH, Kang TW, Jung JH, Kim SJ, Kim KJ. Acute epididymitis in children: the role of the urine test. Korean J Urol. 2013 Feb;54(2):135-8. PMID: 23550228. [PubMed] [Read by QxMD]
Santillanes G1, Gausche-Hill M, Lewis RJ. Are antibiotics necessary for pediatric epididymitis? Pediatr Emerg Care. 2011 Mar;27(3):174-8. PMID: 21346680. [PubMed] [Read by QxMD]
Sakellaris GS1, Charissis GC. Acute epididymitis in Greek children: a 3-year retrospective study. Eur J Pediatr. 2008 Jul;167(7):765-9. PMID: 17786475. [PubMed] [Read by QxMD]
Somekh E1, Gorenstein A, Serour F. Acute epididymitis in boys: evidence of a post-infectious etiology. J Urol. 2004 Jan;171(1):391-4; discussion 394. PMID: 14665940. [PubMed] [Read by QxMD]




Great article that I was able to quickly read and apply while on shift! Thanks for saving my patient unnecessary antibiotics!
Thank you for this blog! Epididymitis Causes
That is a great tip especially to those fresh to the blogosphere.
Brief but very accurate information… Thank you for sharing this one.
A must read post!
When you’re 11, and in that much pain, not to mention very embarrassed for being a naked boy among adult strangers, The placebo aspect alone of the antibiotics is massive, as is getting dressed for discharge. I remember clutching that box of pills for dear life, pulling my pants on and seeing a way out of a confusing and very personal situation, before the first dose. Maybe NSAIDs would work too. Just don’t send him home empty handed with vague medicine recommendations. (Hand the kid a magic hospital-only box of stardust.)
And just because he doesn’t disclose sexual activity, don’t skip on the advice. He can’t tell you. I was very scared when they asked if I was being abused. I was being abused. Trouble is, It sounded like judgement. Also it would have broken my dads heart to hear that, as well as my ballache! (Dad rushed me to ER)
Thank you for this article. It’s the one outlier amongst a sea of articles that recommend antibiotics and it gives me ammo to not just go along. My 11 year old son was diagnosed with this today in the ER. They told us it was uncommon in children and he was going to be put on antibiotics. His urinalysis came back clean, he had no elevated temperature, and has not had any viral infections. I’m pushing back and asking that they actually determine that he has an infection before I just throw him on antibiotics (he’s never had antiobiotics in his life and he’s super healthy).
[…] PedsEMMorsels: Epididymitis in Children […]