Tapping a VP Shunt
The number of technology dependent children that we see seems to steadily be increasing. These technologies can be quite beneficial for the patient, but are associated with potential complications and issues. Ventriculoperitoneal (VP) shunts certainly benefit patients who have hydrocephalus; but how do we handle their issues?
Shunt Components
(Basics – there are a wide variety of different systems, but their basic set up is similar)
- Interventricular Catheter (travels through burr hole in skull)
- Reservoir (between Interventicular Catheter and Valve)
- Valve (several different types – see reference)– allows for unidirectional flow of CSF
- Antisiphon Device and “on/off” device – may be distal to valve
- Distal Tubing that travels from Valve to peritoneal cavity
Most Common Complications
- Infection
- Most commonly within first 6 months after operative placement
- Most common associated risk factor = Age under 3 months
- Organisms : think Skin Flora primarily
- Fever in this period is a problem, but absence of fever doesn’t rule it out!!
- Have a High Index of Suspicion
- Malfunction (Overdrainage or Obstruction)
- May occur at any time
- Obstruction is most common cause of malfuntion
- Obstruction is potentially life-threatening
- Proximal Obstruction causes
- Debris (Choroid Plexus) in shunt
- Fibrosis
- Infection
- Catheter migration into parenchyma
- Distal Obstruction causes
- Kinking or clogging of tubing
- Infection
- Migration of catheter
Signs and symptoms of Malfunction … and also Infection (as you see Infection can cause Malfuntion)
- HA
- Nausea, Vomiting,
- Change in Mental Status (sometimes you have to rely on the parents for this one)
- New neuro finding
- Autonmomic instability
- Coma / Respiratory compromise
- Swelling around the shunt (CSF leaking out around the valve)
- Bulging fontanelle
- Papilledema
- Limited Upward Gaze (Sun-Downing)
OK, so you have a stable patient with a VP shunt who has some concerning symptoms, what do you do?
- Head CT (to help define if there is hydrocephalus vs overdrainage)
- Shunt Series (to image the apparatus for obvious kinks and breaks)
- Consult Neurosurgery for possible VP Shunt tap.
- If the child is stable, the Neurosurgeon should be involved with the decision to tap the shunt and should be responsible for it.
OK, now the child looks really bad and has signs of increased ICP… now what do you do?
- Elevate head of bed
- Intubate? Consider lidocaine and thiopental (even though I love Ketamine, obstructive hydrocephalus and ketamine don’t go well together) and a nondepolarizing paralytic.
- Tap the shunt (feel free to page Neurosurgery… but it isn’t appropriate to let the child’s brain squish just because the Neurosurgeon hasn’t called back or made it in).
-
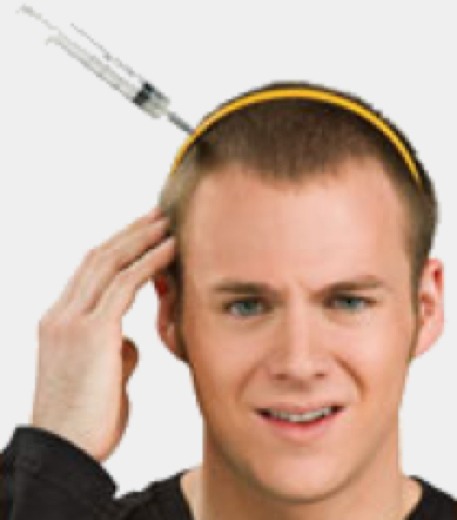
EMERGENT VP SHUNT TAP
- Indication: Severely elevate ICP
- Contraindication: Overlying infection
- How to:
- Informed consent (naturally)
- Review images and identify the shunt reservoir and palpate its location.
- Topical LMX would be nice if you had time… but not necessary in emergency (you are using a 25 Gauge needle… infiltrating with lidocaine would likely be more painful and potentially obscure your landmarks)
- Place patient with CP shunt reservoir in uppermost position.
- Sterile Prep (paramount) – you don’t need to shave the hair, but use the chlorhexidine or iodine to get it out of your way. Use Sterile Drapes.
- Attach 25 G Butterfly needle’s tubing to 3-way stop-cock and manometer.
- Insert butterfly needle into the reservoir. Advancing slowly. Hold manometer at level of the patient’s ear.
- If proximal catheter is not obstructed, CSF will flow into the manometer.
- Pressures above 15mmHg are abnormal (>25 are postiviely correlated with distal shunt obstruction).
- If there is proximal obstruction, there may be no CSF flow or poor CSF flow – now you need the Neurosurgeon to get the kid to the OR.
- If there is elevated ICP, withdraw CSF until pressures are less than 15mmHg.
- Collect CSF slowly as to reduce risk of interventricular bleeding.
- Withdraw needle and hold pressure with sterile guaze for ~2 minutes.
- Complications
- Shunt Infection
- Interventricular hemorrhage
- Shunt reservoir damage
This is certainly not something that you do everyday … and I would discourage you from doing it merely because you think the child has a shunt infection or even a malfunction, but is clinically stable. This should always be discussed with the Neurosurgeon; however, on occasion, you may be the only doc in the middle of nowhere and the kid is bradycardiac and having respiratory issues and has papilledema… then, in that case, get out your 25 Gauge butterfly needle and make a difference!
Key CB, Rothrock SG, Falk JL. Cerebrospinal fluid shunt complications: an emergency medicine perspective. Pediatr Emerg Care. 199 Oct; 11(5):265-73
THANKS TO DR. MCLEAN (click on link to go to Pubmed page for full article):
John Holter’s Shunt


[…] Tapping a VP Shunt on Pediatric EM Morsels […]
hello dear.
i have a 10 years child with VP shunt done in age (5 month) later now days she had headache and vomiting after doctors consult they decide to insert needle and csf out about 30 mm child feel better maybe every 8 hors. but only for one or tow day then child go better and out from hosp.
now this attack happen every month .the doctors say not need replacement shunt .because she is good and say it is on -off shunt
please advice me what can i do ????
Hello,
Obviously, I cannot give out specific medical advice over the internet. I would say, that most often issues like you describe can be resolved by having a specific appointment made to discuss all of your questions openly with your medical providers.
I wish you all the best,
sean
I need mine looked at but my insurance will not cover test what should I do
[…] Unfortunately, VP shunts can have complications… and we have discussed some of them before (Tapping a VP Shunt). The evaluation of a child with a VP shunt who is not critically ill (and not in need of having […]
[…] Tapping a VP Shunt on Pediatric EM Morsels […]
[…] Tapping VP shunts – Pediatric EM Morsels […]