Nail Bed Lacerations

Kids stick their fingers into places where they shouldn’t be, either by curiosity into electrical sockets, (Electrical Injury) or by accident into home and car doors and windows (Subungal Hematoma). It’ll be up to you to put your finger on the problem, diagnose that nail bed laceration, and repair it properly so that the parent tells you that you “NAILED it!” Let’s take a moment to digest a Morsel on Nail Bed Lacerations:
Nail Bed Lacerations: Let’s POINT out a few things
- Fingertip and nail bed injuries are some of the more common hand injuries in kids. [Roser, 1999; Gellman, 2009]
- Jamming or crushing the finger in a door at home is very common, especially for children under 5 years old [Doraiswamy 2000]
- Hand and finger injuries peak in a bimodal fashion during summer and fall and cost over $4.5 billion per year (average of up to $2000 per ED visit). [Lee, 2021]
- Nail bed injuries occur in up to one quarter of fingertip injuries. [Edwards 2019]
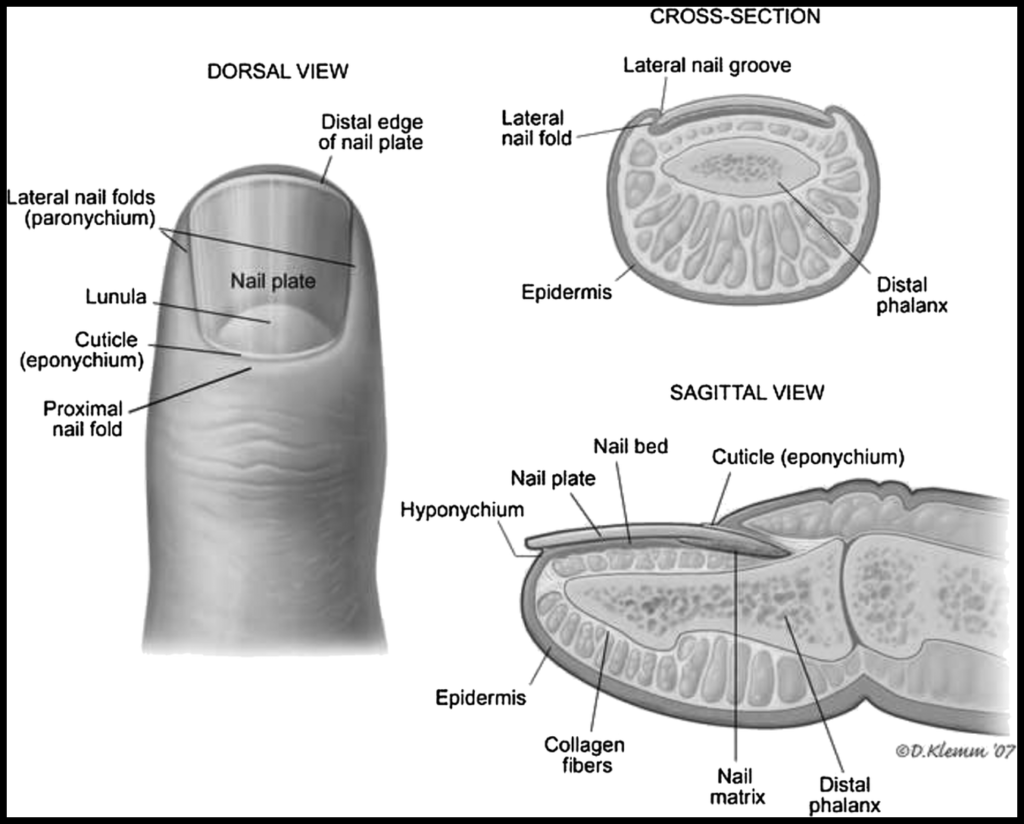
Nail Bed Lacerations: Anatomy Matters
What nailbed anatomy are we working with? [Jones, 2021]
- Perionychium includes the nail, nailbed, and surrounding skin
- Paronychium includes the lateral nail folds
- Hyponychium is the skin distal and palmar to the nail
- Eponychium includes the dorsal nail fold and proximal to nail fold
- Lunula is the white part of the proximal nail
- Matrix has two parts
- Sterile
- soft tissue deep to nail
- distal to lunula
- adheres to nail
- Germinal
- soft tissue deep to nail
- proximal to sterile matrix
- performs nail development
- Sterile
Nail Bed Lacerations: How to Repair
Once you see that your patient has a nailbed laceration, how do you repair it? [Sutijono, 2017; Patel, 2014]
- Digital block with 1% lidocaine
- Clean hand and finger with povidone-iodine
- Wrap with tourniquet for bleeding control
- Remove injured native nail
- Approximate and SUTURE OR GLUE the lacerated nail bed pieces
- 6-0 chromic gut is common
- Cyanoacrylates have been used to glue and avoid sutures
- Replace the native nail to stent open the nail fold -OR-
- Insert a nail-shaped inorganic object, like a piece of the suture packet material
- Suture stent in place through hyponychium with 2 non-absorbable sutures
- Apply antibiotic ointment and loose protective dressing
CUT to the chase! Which is better: sutures or glue?
- Small studies have been done to evaluate the effectiveness of cyanoacrylates in nail bed repairs. [Edwards 2019]
- Comparative studies have not shown a significant difference in final cosmesis or functional ability. [Strauss, 2008; Edwards, 2019; Patel, 2014; Langlois, 2010]
- Stronger evidence and larger studies are desired by some. [Venkatesh, 2020]
- Medical adhesives offer significantly faster repair times. [Strauss, 2008]
- Cyanoacrylates can secure the nail plate into the eponychial fold instead of sutures. [Stanislas, 1997; Richards, 1999]
To antibiose or not to antibiose?
Prophylactic antibiotics are used often depending on the mechanism of injury. [Sutijono, 2017]
- Animal and human bites (Augmentin or non-penicillin alternative)
- Crush injuries (1st gen cephalosporin)
- “Open fractures”– Tuft fracture with nailbed injury (1st gen cephalosporin)
- The benefit of prophylactic antibiotics has not been substantiated in “open fractures,” but is still commonly practiced.
- A systematic review by Metcalfe et al found no difference in rate of infection or osteomyelitis between those who are treated with prophylactic antibiotics and those who were not. [Metcalfe, 2016]
Nail Bed Lacerations: Complications
- Hook nail from advancement of the matrix without adequate bony support [Jones, 2021]
- Split nail from scarred matrix after nail bed injury [Jones, 2021]
Moral of the Morsel
- Nail bed injuries in kids are COMMON!
- Significant nail bed lacerations MUST be evaluated and repaired to avoid bad cosmesis.
- Cyanoacrylates may be as effective as suturing for nail bed injury repairs in children.
- Unless a bite injury necessitates antibiotic treatment, clean injuries including open fractures are not proven to benefit from prophylactic antibiotics.
- Now you can Nail this one!
References
Roser SE1, Gellman H. Comparison of nail bed repair versus nail trephination for subungual hematomas in children. J Hand Surg Am. 1999 Nov;24(6):1166-70. PMID: 10584937.
Gellman H. Fingertip-nail bed injuries in children: current concepts and controversies of treatment. J Craniofac Surg. 2009;20(4):1033-1035. doi:10.1097/SCS.0b013e3181abb1b5
Doraiswamy NV, Baig H. Isolated finger injuries in children–incidence and aetiology. Injury. 2000;31(8):571-573. doi:10.1016/s0020-1383(00)00052-8
Lee A, Colen DL, Fox JP, Chang B, Lin IC. Pediatric Hand and Upper Extremity Injuries Presenting to Emergency Departments in the United States: Epidemiology and Health Care–Associated Costs. HAND. 2021;16(4):519-527. doi:10.1177/1558944719866884
Edwards S, Parkinson L. Is Fixing Pediatric Nail Bed Injuries With Medical Adhesives as Effective as Suturing?: A Review of the Literature. Pediatr Emerg Care. 2019;35(1):75-77. doi:10.1097/PEC.0000000000000994
Jones, MD T. Nail Bed Injury – Hand – Orthobullets. Orthobullets.com. https://www.orthobullets.com/hand/6109/nail-bed-injury. Published 2021. Accessed September 2, 2021.
Patel L. Management of Simple Nail Bed Lacerations and Subungual Hematomas in the Emergency Department. Pediatric Emergency Care. 2014; 30 (10): 742-745. doi: 10.1097/PEC.0000000000000241.
Sutijono, MD D, Silverberg, MD, MMB, FACEP M, Kardon, MD, FACEP E. Nailbed Injuries Treatment & Management: Emergency Department Care, Consultations, Medical Care. Emedicine.medscape.com. https://emedicine.medscape.com/article/827104-treatment. Published 2017. Accessed September 2, 2021.
Strauss EJ, Weil WM, Jordan C, Paksima N. A prospective, randomized, controlled trial of 2-octylcyanoacrylate versus suture repair for nail bed injuries. J Hand Surg Am. 2008;33(2):250-253. doi:10.1016/j.jhsa.2007.10.008
Langlois J, Thevenin-Lemoine C, Rogier A, Elkaim M, Abelin-Genevois K, Vialle R. The use of 2-octylcyanoacrylate (Dermabond(®)) for the treatment of nail bed injuries in children: results of a prospective series of 30 patients. J Child Orthop. 2010;4(1):61-65. doi:10.1007/s11832-009-0218-1
Venkatesh A, Khajuria A, Greig A. Management of Pediatric Distal Fingertip Injuries: A Systematic Literature Review. Plast Reconstr Surg Glob Open. 2020;8(1):e2595. Published 2020 Jan 20. doi:10.1097/GOX.0000000000002595
Stanislas JM, Waldram MA. Keep the nail plate on with Histoacryl. Injury. 1997;28(8):507-508. doi:10.1016/s0020-1383(97)00050-8
Richards AM, Crick A, Cole RP. A novel method of securing the nail following nail bed repair. Plast Reconstr Surg. 1999;103(7):1983-1985. doi:10.1097/00006534-199906000-00028
Metcalfe D, Aquilina AL, Hedley HM. Prophylactic antibiotics in open distal phalanx fractures: systematic review and meta-analysis. J Hand Surg Eur Vol. 2016;41(4):423-430. doi:10.1177/1753193415601055


Keep up the great work guys!! Love reading these and helping others enjoy and learn from them!!! Miss you guys!
THANK YOU!!
Feel free to come back!
-Sean
I still have not unsubscribed to your mailings as you do such a great job, and although I “retired” from EM 6 months ago to work in hospice, I still enjoy reading what you send. Regarding nail bed lacerations, let me share a thought or two. Firstly, as doctors we are, more or less, human beings. As such we act in our own best interest and at times this includes, if not outright lies, at least a somewhat fluid relationship to the facts. Imagine a fingertip injury. Not pretty to begin with, certainly no better after the nail, or what remains of it, is “gently” avulsed. Now you’re in up to your waist, looking at a bleeding mass of mangled hamburger, a possibly screaming patient, and a parent or nurse looking over your shoulder. With ridiculously small 6-0 suture you take a bite here and there, tie a knot or two, and try to move on. You then chart how the laceration of the nail bed was well approximated using 3 interrupted 6-0 sutures, when in reality nothing this exact really happened. I would bet that most “nail bed repairs” are something less than that. About 15 years ago, I stopped trying to engage in what I viewed as a relatively futile effort at nail bed repair (in kids and adults). Here is my algorithm: If the finger is badly mangled, send it to plastics. Lacs accessible to repair without messing with nail bed are repaired. Leave the nail, or what remains of it in place. Vaseline gauze, wait. I have spent 20+ years in small town EDs, so have the luxury of frequent follow up, sometimes seeing the same patient multiple times over many years. I have been pleasantly surprised how many fingers have healed wonderfully. I have had no feedback reporting complications using the above method. I realize that the medical literature may not support this technique, but I wonder if the literature accurately reflects what is truly going on. I think many of the good outcomes reported following nail removal and primary repair and really good outcomes despite suspect treatment.
Keep up the good work,
Mike
Mike,
First of all, thank you for following and the support!
Secondly, I agree with your sentiment… repairing nail bed injuries sucks. Sewing paperthin, friable tissue is one of my least favorite things to do… and is why I like the Dermabond option. Clearly, there are some that have other concurring injuries that require sutures… but if it is isolated, I use glue.
Long ago I was taught that a large subungual hematoma was an indication to remove the nail to “inspect” the nail bed… I stopped doing that a long time ago. If the nail plate is intake, I leave that alone… except for trephination.
Stay well,
sean