Pyloric Stenosis
We have discussed vomiting a lot (we just can’t get away from it sometimes!). We covered “simple” issues like emesis/diarrhea and therapies for dehydration. We have also covered more ominous conditions like intussusception, necrotizing enterocolitis, and Inborn Errors of Metabolism. All of these conditions deserve our attention and frequent consideration when evaluating the child with vomiting; however, there is one entity that is commonly considered, often encountered, and frequently the topic of test questions: Pyloric Stenosis.
Pyloric Stenosis
- Infantile Hypertrophic Pyloric Stenosis is the most common condition that requires surgery in infants.
- Etiology is still unclear. Likely multifactorial (genetics, tob exposure, bottle feeding vs breastfeeding, etc).
- Incidence = 2-5 per 1,000 births per year!
- Male:Female = ~5:1
- Ages
- The mean age at diagnosis was once 5.9 weeks.
- Now mean age is 4 – 5.5 weeks.
- Mean duration of symptoms prior to ED evaluation in one study = 5 days.
Pyloric Stenosis Anatomy
- The pyloric ring is not clearly distinguishable from the pyloric antrum and the duodenal cap.
- The channel is characterized by thickened muscle and the canal is filled with compressed and redundant mucosa, which can protrude into the gastric antrum.
- This leads to gastric outlet obstruction.
Pyloric Stenosis Presentation – Classic
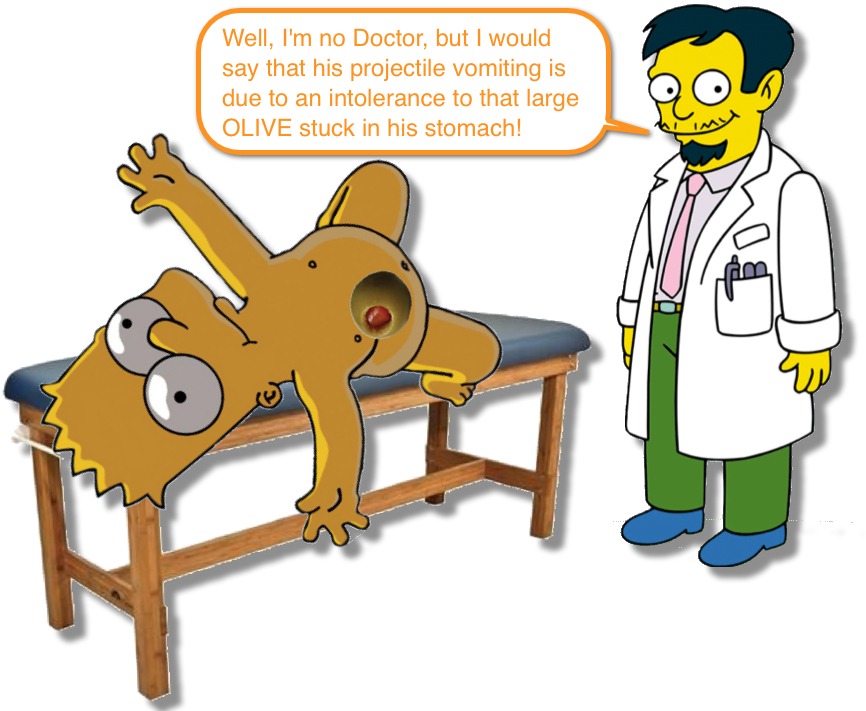
- Everyone has an image of what the classic infant with Pyloric Stenosis looks like:
- Child has evidence of failure to thrive and appears wrinkled and dehydrated. (see Gross Growth Estimates for reference)
- The kid has a intense, inconsolable cry as he/she is starving and really wants to eat. Often has evidence of sucking pads on the hands/wrists.
- The family describe a voracious appetite, but feeding is followed by “projectile vomiting” that is nonbilious.
- On exam you can feel an “olive” in the RUQ and can see “peristalic waves.”
- Labs show hypochloremic, metabolic alkalosis with hypokalemia.
- If your test has a 4 week old with projectile, nonbilious emesis who appears hungry and has failure to thrive, the answer is Pyloric Stenosis.
- But… as we are all aware… things are just not that simple.
- The diagnosis, historically, is one made clinically; however, today, Ultrasound allows us to diagnosis pyloric stenosis earlier; often before the classic findings are apparent.
Labs?
- We love to pimp residents and students about the electrolyte abnormalities seen with Pyloric Stenosis… it is a great way to learn some basics.
- With early diagnosis, however, NORMAL lab values are the most common lab finding in cases of Pyloric Stenosis.
- Metabolic Alkalosis was found in older infants.
- Bottom line… normal labs do not rule-out Pyloric Stenosis.
The Olive!
- Palpation of the hard mass of muscle (AKA the Olive) is diagnostic… but difficult.
- Requires a calm and cooperative child (difficult to achieve in a starving kid).
- Requires time to achieve that calm and cooperative child.
- The distended stomach can obscure the olive.
- Early on in the disease course, the child may still have normal subcutaneous fat, also obscuring the olive.
- Are our clinical exam skills declining?
- Studies in the ’70’s showed detection of the Olive to be successful in 87% of infants with pyloric stenosis.
- Only 49% of the time was the Olive noted in a study looking at 1988-1991.
- In 2013, a study found that the Olive was noted in only 39% of Pyloric Stenosis cases.
- This is not a commentary on our “poor physical exam skills,” but rather on our ability to diagnosis the condition earlier with U/S.
- While some have described methods to improve your palpation of the olive (like sedation! or NG tube placement to decompress the stomach), these seem extreme when U/S is so easy.
Bilious Emesis?
- Ok… first of all… Bilious Emesis in a neonate is a surgical emergency until proven otherwise! Sepsis would also be high on the DDx.
- But, every textbook that describes Pyloric Stenosis associates it with “non-bilious emesis” as if bilious emesis rules-out Pyloric Stenosis.
- While bilious emesis is a rare presentation of Pyloric Stenosis, its presence does NOT rule-out pyloric stenosis.
- Two studies recently have shown that Pyloric Stenosis can be associated with bilious emesis.
- It is Rare – 1.4 % – 4 %
- Pts with bilious emesis and Pyloric Stenosis had statistically significant smaller pyloric thickness measurements.
- Two studies recently have shown that Pyloric Stenosis can be associated with bilious emesis.
- While bilious emesis can be seen with Pyloric Stenosis, the imaging modality of choice would by an Upper GI to look for malrotation!
Imaging for Pyloric Stenosis
- Currently, the two valid methods for diagnosing Pyloric Stenosis are Upper GI and Ultrasound.
-
Upper GI
- The canal is outlined by a “string” of contrast going through the elongated pyloric channel = “String Sign“
- May also see several linear tracks of contrast separated by redundant mucosa = “Double-Track Sign“
-
Ultrasound
- The length of the hypertrophied canal is variable (as little as 14 mm to 20 mm).
- The muscle thickness also is variable (3.0 – 4.5 mm). Should be > 3mm throughout the examination.
- The overall morphology is more important than the numerical values and the real-time images of movement of the structures is vital.
- Can often see the mucosa sliding within the canal.
Bottom Line: Currently, patients present earlier and are diagnosed more readily with simple techniques and this has lead to reductions in the frequency of metabolic disturbances, dehydration, and starvation. So the “classic” findings of Pyloric Stenosis are becoming less commonly found.


[…] Fox gives an overview of pyloric stenosis in Pediatric EM Morsels this week. Bilious vomiting does not exclude pyloric stenosis – read […]