Sentinel Bruising & Abusive Injury
A common theme amongst the Ped EM Morsels is remaining vigilant while maintaining a reasonable approach to the care of children. Many devastating conditions can be quite subtle in their initial presentation. Last week, a prior PEM graduate from Carolinas Medical Center, Dr. Simone Lawson joined me to chat about a potentially devastating condition that can easily be, and unfortunately is, often missed at first presentation: Child Abuse. While discussing this critically important topic on EMGuideWire’s Core Concepts (take a listen and consider subscribing – it’s free!) with our Child Protection expert, Dr. Pat Morgan, a useful tool was brought up to help us all not miss the subtle presentation of child abuse. I wanted to reiterate it here. Let’s take a minute to remember the importance of Sentinel Bruising and Abusive Injuries in Children:
Bruising in the Peds ED
- Bruising is commonly seen in the Pediatric ED. [Pierce, 2016]
- Infrequently is it related to a medical condition (ex, Hemophilia, ITP).
- Most often it is related to traumatic complaints (Gravity works!).
- Non-accidental Trauma… is Trauma… but can be overlooked easily.
- Bruising may be the “sentinel” sign of non-accidental trauma in a child. [Pierce, 2017; Pierce, 2017; Pierce, 2009]
- It is known to be under-appreciated in those children who later are found to be severely injured or killed.
- 28-64% of children who sustain severe physical abuse were found to have had a prior “sentinels” bruise. [Pierce, 2017; Pierce, 2017]
Bruising: Looking for Red Flags
If bruises occur commonly, are often due to explainable accidents, and we often overlook them as they don’t require specific therapy, BUT they can also be the first clue indicating physical abuse is occurring, how can we reasonable remain vigilant?
Look for well known Red Flags!
- Bruising characteristics that are concerning for abuse: [Pierce, 2016; Pierce, 2010]
- Number of Bruises
- More than 3 bruises from one event are uncommonly due to accidents (unless from falls down stairs or MVCs)
- Having 5+ bruises is very concerning.
- Location of Bruises
- Posterior surface (Torso, buttocks, posterior legs)
- Front AND Back of the body from reported single event is concerning!
- Ears
- Neck
- Hands
- Chest
- Genitals
- Type of Bruises
- Petechial bruising
- Bruises with Patterns
- Linear
- Appearance similar to a known object
- Number of Bruises
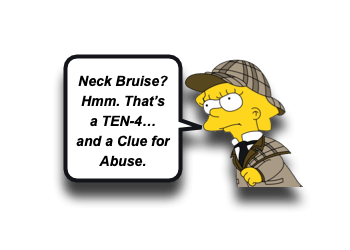
- TEN – 4 FACES P [Pierce, 2016; Pierce, 2010]
- In children less than 4 years of age, bruises on these areas raise concern for physical abuse:
- Trunk
- Ears
- Neck
- ANY BRUISE on a child less than 4 months of age is concerning!
- It’s always good to recall your Developmental Milestones!
- “Kids that don’t cruise rarely bruise.” [Pierce, 2009]
- Infant homicide rates are highest in the first 4 months of life.
- Additionally, bruises on these areas should also raise concerns:
- Frenulum (tear or bruising)
- Auricular area
- Cheek
- Eyes
- Sclera
- Patterned bruising is always concerning!
- In children less than 4 years of age, bruises on these areas raise concern for physical abuse:
- Ask more questions:
- If a possible “sentinel” bruise is discovered, ask more questions.
- If a plausible cause of the bruising cannot be discerned, then non-accidental trauma should be high on the list of concerns.
- Having a confirmed accident in a public setting that can be attributed to the bruise can be reassuring. [Pierce, 2010]
- All you need is a concern for abuse (you don’t need definitive evidence) to report this concern to protective services and resources.
Moral of the Morsel
- Put them in Gowns (or at least look at the skin)! Every encounter is an opportunity to ensure each child is safe and well cared for.
- Remain vigilant! Look for Red Flags of abuse (TEN-4 FACES P).
- Ask more questions. Does the reported event make sense to have caused bruises on the front AND back of the Torso??

