White Eye Blowout
Kids have big heads relative to their bodies. Unfortunately with relatively big heads comes many traumatic injuries – think pediatric facial fractures, nasal fractures, tongue lacerations, ear lacerations, and dental injuries. The eye tends to unfortunately bear the brunt of some trauma, too. I’m looking at you hyphema and traumatic glaucoma!
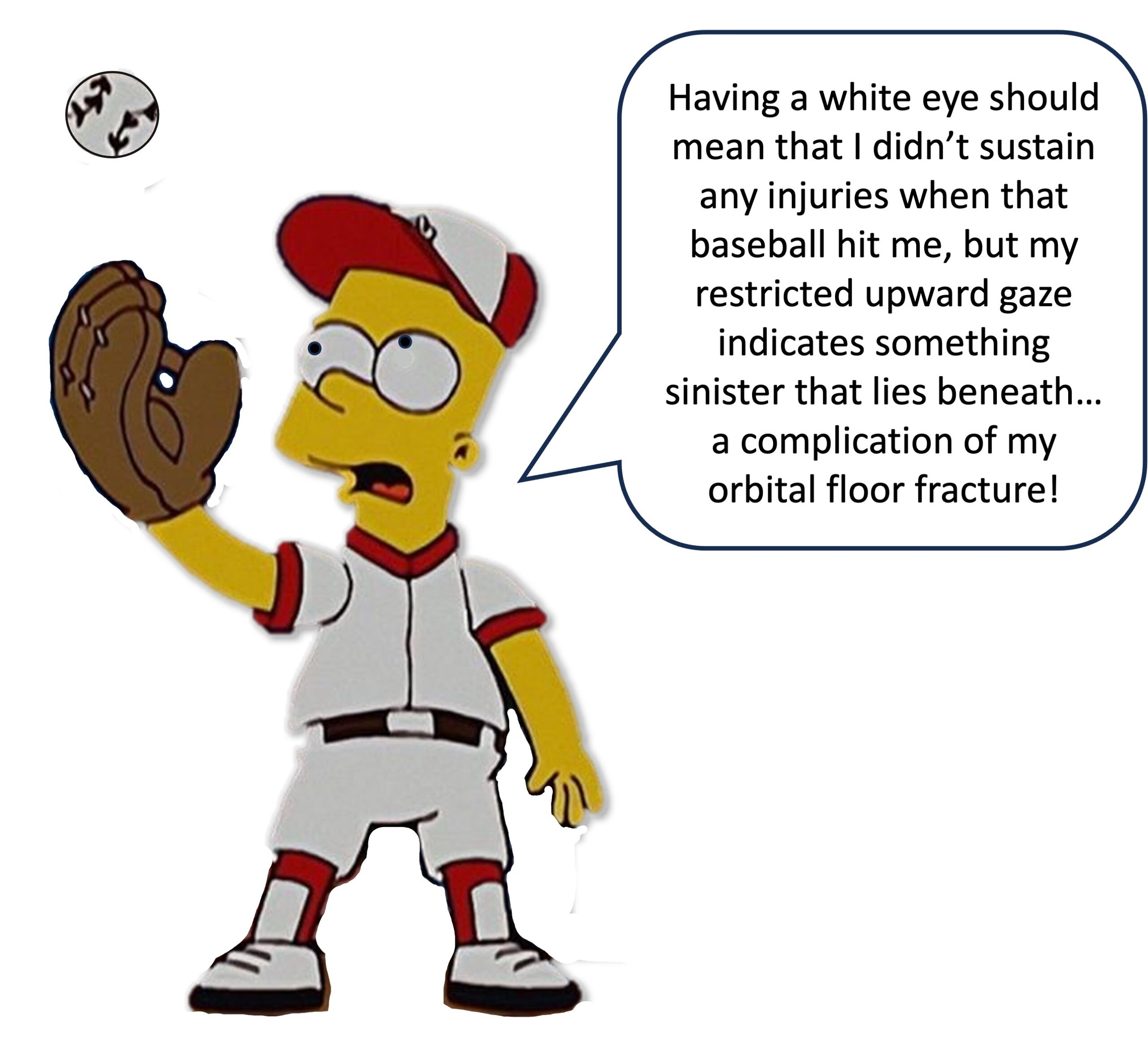
There are also some injuries that may be difficult to appreciate on first glance at a patient. There may be other larger, more distracting injuries that have pulled your attention. Vigilance is key, as is a very thorough physical exam to ensure you don’t miss these crucial diagnoses, such as nasal septal hematomas, frenulum tears, open globe injuries (which can be subtle), and mandible fractures. One particularly elusive injury presents with a “White Eye” Blowout since there is no outward indication of soft tissue injury. This is a complication of orbital floor fractures when soft tissue gets trapped by the fracture fragments. Let’s talk further about the “White Eye” Blowout.
White Eye – Basics
- Orbital floor blowout fractures comes from increased pressure to the eye from blunt direct injury [Balaraman 2021, Amarath-Madav 2022, Hakkou 2024]
- Increased pressure causes bowing and breaking of thin orbital floor bone
- In kids, this often causes linear rather than comminuted fractures
- Kid bones are still somewhat elastic, and the intact side of the bone springs back, acting like a trap door
- Soft tissue can get caught in this trap door
- Pediatric facial fractures <15% of all facial fractures [Jordan 1998, Joshi 2011]
- Orbital blowout fractures 20% of pediatric facial fractures (range 7-41%)
- Often in adolescents, but can happen in younger children
- Usually during sports, from a fall, or during an assault
- “White eye” blowout fractures, in particular, show no other outward signs of injury!
White Eye – Presentation and Exam
- After an injury to the face or head, often a sports injury
- Patient may not have outward signs of soft tissue injury such as ecchymosis, tissue edema, or conjunctivitis (Hence, “white eye”) [Balaraman 2021]
- But they do have:
- Restricted upward gaze
- May have nausea or vomiting, which is also common with head injuries
- Diplopia
- Lack of enophthalmos
- Eye pain
- May have unexplained bradycardia (oculo-cardiac reflex)
- Be vigilant! Symptoms can mimic typical head trauma and increased ICP, and this is easily missed on initial exam [Tarbet 2021]
- One study showed up to 33% of pediatric cases were missed or misdiagnosed
White Eye – Diagnosis
- Have a high suspicion with a good physical exam with unilateral restriction of gaze
- Non-contrast CT scan (need high resolution) [Amarath-Madav 2022]
- May only see a very subtle fracture line
- Look for entrapped tissue
- Look at coronal or sagittal views
- Tear drop sign when entrapped tissue is seen herniating through fracture [Hakkou 2024]
White Eye – Treatment
- Previous thought was conservative management for 4-6 months [Jordan 1998]
- “Watch and wait”
- Some recommended waiting for 2 weeks before operating
- This is sometimes the treatment for adults who don’t get entrapment of tissue as often
- This is another example of the anatomy and physiology of children mandating a different approach.
- Now urgent or emergent surgery is recommended for children [Jordan 1998, Egbert 2000]
- Pediatric patients were found to rarely have spontaneous resolution
- Some had permanent motility restriction when surgery was delayed
- Usually go to OR with 24 hours
- Emergent OR for surgical management if showing signs of oculo-cardiac reflex bradycardia
- Often mesh is placed to prevent re-herniation of inferior rectus, fat, and other soft tissue [Balaraman 2021, Hakkou 2024]
White Eye – Complications
- Oculocardiac or oculovagal reflex (OCR) = bradycardia + nausea, vomiting [Balaraman 2021, Amarath-Madav 2022]
- Also known as the Dagnini-Aschner reflex, or “Aschner reflex”
- Trigeminal-Vagus nerve reflex arc is triggered by stretch receptors of short and long ciliary nerves
- The trigeminal sensory nucleus is activated, and sends impulses to the visceral motor nucleus and subsequently the vagus nerve
- Vagus nerve stimulation acts on the SA and AV nodes, causing bradycardia, which can be profound
- Worsened by upward gaze, puts pressure and stress on the trapped soft tissue
- A literature review showed that 77% who presented with this OCR had orbital floor fractures
- 70% had muscle entrapment
- Nausea and vomiting
- Diplopia (20%)
- *Usually* resolves after surgical reduction of entrapped tissue
- Can persist for weeks to months after surgery
- Permanent or long term ocular mobility problems
- Balaraman reported one case where diagnosis was delayed 9 days
- Diplopia resolved after 45 days
- Had permanent residual restriction of upward gaze [Balaraman 2021]
- Balaraman reported one case where diagnosis was delayed 9 days
- Permanent vision disturbances
- One case report of a Volkmann’s type of contracture of the inferior rectus muscle [Smith 1984]
- Delayed release and prolonged tissue incarceration could reduce perfusion to the muscle and cause scarring [Balaraman 2021]
- Periorbital edema
- Parasthesia of maxillary portion of trigeminal nerve [Amarath-Madav 2022]
- Thought to be from irritation of infraorbital nerve when fracture disrupts infraorbital canal
Moral of the Morsel
- Have a KEEN EYE for subtle exam findings! Symptoms of a white eye orbital blowout fracture can be subtle and easily missed.
- Do a double-take to avoid double vision! Prompt diagnosis is key to avoid long term issues like diplopia, restricted upward gaze, and muscle scarring.
- Don’t cry- look for the teardrop sign! High resolution CT scan is best for diagnosis. Fractures are hard to see, but look for the entrapped soft tissue.
- Be still my heart! The oculocardiac reflex can cause severe and life-threatening bradycardia. Pay attention to the vital signs.
- Cut to cure! Prompt surgical intervention relieves entrapped tissue and reduces complication rates.
REFERENCES
- Jordan DR, Allen LH, White J, Harvey J, Pashby R, Esmaeli B. Intervention within days for some orbital floor fractures: the white-eyed blowout. Ophthalmic Plast Reconstr Surg. 1998;14(6):379-390. doi:10.1097/00002341-199811000-00001 {PMID 9842557}
- Joshi S, Kassira W, Thaller SR. Overview of Pediatric Orbital Fractures. Journal of Craniofacial Surgery. 2011; 22 (4): 1330-1332. doi: 10.1097/SCS.0b013e31821c9365.
- Balaraman K, Patnaik JSS, Ramani V, et al. Management of White-Eyed Blowout Fracture in the Pediatric Population. J Maxillofac Oral Surg. 2021;20(1):37-41. doi:10.1007/s12663-020-01393-0 {PMID 33584039}
- Egbert JE, May K, Kersten RC, Kulwin DR (2000) Pediatric orbital floor fracture: direct extraocular muscle involvement. Ophthalmology 107(10):1875–1879 {PMID: 11013191}
- Smith B, Lisman RD, Simonton J, Della RR (1984) Volkmann’s contracture of the extraocular muscles following blowout fracture. Plast Reconstr Surg 74(2):200–216 {PMID: 6463145}
- Amarath-Madav R, Adamkiewicz D, Bigler D, Yu JC, Lima MH. White-Eyed Orbital Blowout Fracture With Oculocardiac Reflex Secondary to Extraocular Entrapment in a Pediatric Patient. J Craniofac Surg. 2022;33(7):e767-e771. doi:10.1097/SCS.0000000000008713 {PMID: 36109010}
- Hakkou Z, El Zouiti Z, Elayoubi F, Tsen AA. Pediatric trapdoor fracture of the orbital floor with Tear-Drop sign: A case report. Radiol Case Rep. 2024;20(3):1403-1405. Published 2024 Dec 19. doi:10.1016/j.radcr.2024.11.068 {PMID: 39898335}
- Tarbet C, Siegal N, Tarbet K. White-eyed blowout fracture with muscle entrapment misdiagnosed as increased intracranial pressure: An important clinical lesson. Am J Emerg Med. 2021;48:375.e1-375.e3. doi:10.1016/j.ajem.2021.03.060 {PMID: 33867194}
- Prasad C, Arulmozhi M, Balaji J, Nisha MPN. White-Eyed Blowout Fracture. Ann Maxillofac Surg. 2020;10(1):217-219. doi:10.4103/ams.ams_150_19 {PMID: 32855945}
- Yew CC, Shaari R, Rahman SA, Alam MK. White-eyed blowout fracture: Diagnostic pitfalls and review of literature. Injury. 2015;46(9):1856-1859. doi:10.1016/j.injury.2015.04.025 {PMID: 25986667}

