Acholic Stool
 There are many interesting complaints that we encounter in the Emergency Department. Many make you scratch your head (how did they get that FB in the Ear?) and others will challenge you (how do I get this fish hook out of the kid’s face?), but one thing is always true; the guardians of neonates worry about A LOT!! This, I believe, is appropriate. I would rather a new parent be more careful rather than careless and cavalier. Plus, you can never trust a neonate! In addition to the numerous concerns about formula and development, many parents will get worried about the color of the child’s stool. (How delightful. Now we have to talk about poop.) Unfortunately, you can’t just dismiss this concern, as it could be a problem. Let us QUICKLY discuss one of the colors that should grab your attention – Acholic Stool:
There are many interesting complaints that we encounter in the Emergency Department. Many make you scratch your head (how did they get that FB in the Ear?) and others will challenge you (how do I get this fish hook out of the kid’s face?), but one thing is always true; the guardians of neonates worry about A LOT!! This, I believe, is appropriate. I would rather a new parent be more careful rather than careless and cavalier. Plus, you can never trust a neonate! In addition to the numerous concerns about formula and development, many parents will get worried about the color of the child’s stool. (How delightful. Now we have to talk about poop.) Unfortunately, you can’t just dismiss this concern, as it could be a problem. Let us QUICKLY discuss one of the colors that should grab your attention – Acholic Stool:
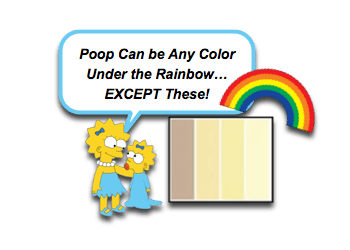
Acholic Stool: Colors of the Rainbow
- Stool color can vary drastically with patient age and diet.
- Stools of healthy breastfed infants are often “daffodil” yellow.
- Stools of healthy formula-fed infants are often “mustard” yellow.
- Certainly, medications and other ingested chemicals / dyes can also affect the stool color.
- Most often the exact color is inconsequential, but we should be mindful of:
- Black and sticky (aka, melena)
- Red and/or maroon (ill-appearing infants with bloody stool warrant concern!)
- Acholic (aka, pale)
- One or two pale stools should not lead to massive freak out!… but persistent acholic stools do warrant evaluation.
- Does not represent one color, but is a spectrum. [Bakshi, 2012]
- “Cream cheese”
- “Uncooked pastry”
- “Manila envelope” (yes, we can describe things in terms that aren’t food related!)
- Dark urine can obscure the stool’s true pale coloration (just to complicate things more). [Bakshi, 2012]
Acholic Stool in Neonate: The Concern
- Biliary Atresia or other cholestatic disease is the biggest concern with acholic stools.
- There are many potential conditions, like neonatal hepatitis that require evaluation.
- Don’t forget other metabolic conditions that stress the body like Sepsis, Hypothyroidism, Galactosemia, and panhypopituitarism.
- Biliary Atresia:
- Most common cause of neonatal cholestasis that requires surgery [Agin, 2016; Bakshi, 2012]
- Characterized by destruction of the hepatic biliary system leading to biliary cirrhosis.
- The condition can be overlooked initially as the infants are generally well appearing.
- Early detection is critical!
- A Kasai procedure has good success rates if performed early.
- Later referral, after cirrhosis has develop, will often lead to liver transplantation.
Acholic Stool: A Significant Clue!
- Traditionally, biliary atresia is thought of when jaundice lasts longer than 2 weeks of life or with acholic stool and/or dark urine.
- After evaluating many potential clues to differentiate patients with biliary atresia from other cholestatic disease:
- Early development jaundice is more commonly seen in biliary atresia. [Agin, 2016]
- The presence of acholic stools was the most sensitive characteristic. [Agin, 2016]
Acholic Stool: Not as Easy as You Think
- So why are we doing a Morsel on Acholic Stool… seems easy… if stool is super pale, than check for biliary congestion…
- But, experienced providers’ (RN and MD) ability to discern acholic stool is not good enough to rely on our unaided visual inspection alone. [Bakshi, 2012]
- There are several tools that exist that can be helpful:
- Stool Cards / Charts have been found to be useful.
- Help with early detection.
- See example stool chart
- See another stool card
- iPhone App (PoopMD) uses RGB hexcodes to discern the acholic stool. [Franciscovich, 2015]
- iPhone App (Baby unchi) [Hoshino, 2017]
- “Baby Poop” app – only available in Japan right now
- Uses machine learning processes to recognize concerning stool colors (if we are using artificial intelligence for this… you know it is serious!).
- Stool Cards / Charts have been found to be useful.
Moral of the Morsel
- Most colors are fine… but not all! Pay attention to the acholic stool complaint.
- Don’t rely on your eyes… even if you have “perfect vision!” Use a stool card/chart!
- If it is acholic, don’t miss the opportunity to save a liver! Check urinalysis, fractionated bilirubin, and LFTs.


why kasai surgery are so complex and dangerous and it was never enhanced since original invention 70 year ago maybe engineer could assist surgeon to enhance the procedure as the surgeon lacks creative thinking
[…] Fox at Pediatric EM Morsels has some colorful crap you need to know. […]