Fontan Complications
Fontan Complications
As more and more children are having successful surgical procedures to compensate for congenital heart disease, the likelihood that one of these post-operative heart patients will present to your ED increases. It is necessary for us to stay aware of not only the basic congenital anomalies, but also the potential repairs and those repairs’ complications.
There are several surgical options for the various congenital heart lesions, but the Fontan is the one that has the longest list of serious complications.
The Fontan Procedure
- The Fontan is the most common procedure for congenital heart disease after the age of 2yrs.
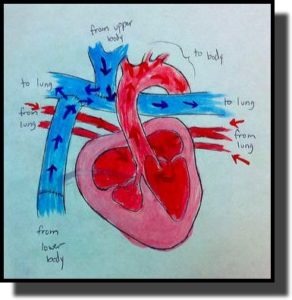
- Refers to any surgical procedure that leads to systemic venous blood flow bypassing the heart and draining directly to the lungs.
- Used in patients with single ventricle and/or pulmonary outflow obstruction, like:
- Tricuspid Atresia
- Hypoplastic left heart syndrome
- The procedure connects the inferior and superior vena cava directly to the right pulmonary artery… such that no ventricular contraction drives pulmonary flow.
- As you can image, the procedure leads to drastic hemodynamic and oxygen saturation changes, so it often is done in stages to help reduce complications.
- Initially a shunt (B-T) is placed between the Subclavian artery and the Pulmonary artery.
- Between 4-12 months a Hemi-Fontan (or Bi-Directional Glenn) is done (SVC connected to Pulm Art).
- The total Fontan is often completed between 1 and 5 years of age.
Possible Complications (abridged)
While this procedure has significantly improved the life expectancy for these children (now we actually see Adult Congenital Heart Disease patients), it can also produce several significant complications.
Gersony WM. Fontan Operation after 3 decades: What we have learned. Circulation. 2008; 117: pp. 13-15. Woods WA, McCulloch MA. Cardiovacular Emergencies in the Pediatric Patient. Emerg Med Clin N Am. 2005; 23: pp. 1233-1249.
- “Pump Issues”
- Arryhthmias & Sudden Death
- May occur shortly after procedure or can occur later in adulthood.
- Some will require surgical intervention for refractory arrythmias.
- Progressive exercise intolerance.
- Ventricular failure
- Vascular Issues
- Thombi and emboli
- Pulmonary (75%) and Systemic systems (25%)
- There is no consensus about daily anticoagulant therapy, but most will have some form of it.
- Stenosis or dilation of the anastomosis sites or conduits.
- Collateral vessel development
- Pulmonary AVM
- Aortopulmonary collateral vessels
- Leads to Shunts
- Elevated central venous pressures
- Venous congestion.
- Cirrhosis, liver failure
- Portal hypertension, Ascites
- Restricted Lymphatic drainage
- Pleural Effusions
- Pericardial Effusion
- Chylothorax
- Protein Losing Enteropathy
- Deserves separate consideration!
- There is a 50% mortality within 5 years of its diagnosis.
- Multiple therapies (which points to poor understanding of it).


My son had his fontan when he was six years old and he is now 35 years old he is experiencing heart failure right now and I don’t know what they should do to treat it. We live in a small town and have to travel for 3 hours to even reach a hospital who can take care of him right. if we take him to the emergency room where we live they don’t know what to do with him they fly him down to UCSF or they just send him home cuz they don’t know how to treat a single ventricle patient. This is very frustrating and scary my son experiences extreme panic attacks and extreme anxiety over this condition for many years he has been afraid to go to sleep at night cuz he’s afraid he won’t wake up again he has four children.
my daughter had the Fontan 2000 at 16 year old and now she 35 years and is having all those issue. Possible Complication she is having them and Children Medical Center Hospital said nothing else they can do for her. She the longest living Fontan
I’m 39. I had my Fonton in 1990.
Hi Sam my name is Kathy Oliver and my son had his fontan done when he was six and he’s 35 now I just wondered how your health is doing now?
So much written on the physical side effects of Fontan.
Yes, I survived pleural effusions, PLE, Severe bronchitis, pericarditis, stent in IVC with the non fenestrated, hemi-fontan, fontan. My liver is being monitored too.
What about the panic attacks, and migraines? What are your other patients using? My sertaline isn’t working.
[…] Congenital heart disease […]
First of all I would like to thank you for the article and information that you have provided me with, just to give you a little insight into my son’s situation his diagnosis are alot to mention right-
I came across this site this morning by chance and it brought upon an abundance of curiosity and worry concerning my son who is 10 1/2 yrs old now. He had the Fontan Procedure when he was a baby first surgery at 1 day old, second at 4 1/2 months old and the last surgery when he was 2 1/2, thankfully they did not insert a shunt otherwise he would had died due to way to much blood flow being dumped. I know with all surgeries that there is chances for complications that may arise and could possible happen. I guess what concerned me the most would have to be the limit of information on just exactly the complications that could occur and what exactly to be aware of as he ages. Continuous care with a Cardiologist of course is a given but I was never aware of the possibilities that could arise when he got older. He was on a ventilator after his first surgery that shook the bed as part of his treatment, deciding whether or not to flip him over during this process became very nerve racking because they constantly were telling us that if they turned him too soon it could go really bad or if they didn’t turn him soon enough it could be even worse then that. Weaning him off of it was like taking a 1/2 baby step forward two adult steps backward and finally after coughing up the tube shoved down his throat for over a month for the second time they finally took him off of it and said oh well i guess his lungs weren’t as sick as we thought they were. His final surgery was last year June 2012 in which they inserted a AMPLATZER Occluder a NON-FERROMAGNETIC/ M.R.I. COMPATIBLE to 3.0T because the hole had no closed in the time they had set previously. Until this time his 02 saturation never went about the mid 80’s where now he is at 90-sometimes 93. The last thing that I want to think of is that he will have even more extensive complications in his future after undergoing this procedure already, he is still unable to play as a normal child due to over exerting himself that causes him to become very fatigued easily not to mention the mental, emotional and learning disabilities damages that all this has caused him. Not to mention having 4 surgeries on his mouth to repair his cleft lip and palate.
I really appreciate your story! Thank you!
Great topic Dr. Fox. Would it be possible to comment on mechanical ventilation management in these patients? Aside from trying to avoid intubation, from what I understand, it’s necessary to minimize PEEP, create short inspiratory times and low inspiratory pressures as positive intrathoracic pressure essentially stops blood flow to the lungs. This may be something that the ED physician has to relay to the RT adjusting the settings on the ventilator.
Dr. Keller,
Great question! You are correct in noting that ventilation management of a patient with CHD (either before or after repair) deserves specific attention. Additionally, these considerations should be made even if you are performing sedation. While this likely requires a dedicated Morsel, what I will say is that Oxygen is a medication and needs to be used judiciously in the patient with CHD as it will cause vaso-dilation and lead to improved pulmonary blood flow and subsequent increases in Pox, but will “steal” blood from the systemic system and can decrease peripheral perfusion.
Additionally, they are very sensitive to alterations in preload, which increased intrathoracic pressure will influence. While this is even true for patients without CHD, it is going to require more attention and constant consideration with balancing the pulmonary and systemic systems in the patient with CHD.
While I agree that you should always utilize your resources… I think that it is imperative that we do not ignore the ventilator… do not give responsibility to managing this crucial part of patient care completely to the RT. I would include the RT in your management decisions, but this part of the patient’s management is in need of your expert opinions.
Below is a nice article also.
Thank you for your comment!
Hope all is well,
sean
Lovell, A.T., Anaesthetic implications of grown-up congenital heart disease. Br J Anaesth, 2004. 93(1): p. 129-39.
Note that the picture is of HRH not HLH but still single ventricle physiology. An ASD or fenestration is needed for mixing at the atrial level. Also the conduit from the inferior vena cava to the RPA typically will have fenestrations placed into the RA to allow for better pressure equilibration.
When a child presents with Single ventricle physiology one of the key elements to figure out is what teh Qp/Qs ration is. If their Oxygen saturation is higher than usual then this is likely >1 and pulmonary overcirculation with systemic undercirculation may be the issue. The goal may be to decrease pulmonary circulation by increasing PVR and decreasing SVR. This may even require a PA band but often can be achieved by limiting Oxygen and hypovenitilating the child, both increased PVR.
The opposite is true if Qp/Qs is <1. Here you want to typically increase pulmonary circulation by sedation, hypervenitilation, increased oxygen tension and potentially nitric oxide.
Oversimplification but illustrates the single ventricle issues with relative flow that must be considered.
Dr. Cordle,
Thank you for the thorough comment. Naturally, the picture is completely over-simplistic… but that is why I liked it (I am simple). There are so many variations of the Fontan (extra-cardiac conduits, intra-cardiac conduits, fenestrations, no fenestrations, etc). I think that this is why many of us have our brains lock up on the subject… plus then you add in the various non-descriptive names (ex, Glen, Fontan, BT Shunt, etc).
As for the fenestrations… it appears that they help decrease complications initially after the surgery, but many are now actually closing the fenestrations later on. So, it is important for us to inquire as to whether this was done or not. The article that is cited from Circulation is a nice review of some of the trends that have occurred over the past 3 decades.
Thank you Dr. Cordle! By the way, your ACEP talks were excellent!
-sean