Ketamine and Laryngospasm

Ketamine. It sounds cool. It works great. It makes many of my shifts easier. Sounds perfect!! Let’s be honest, if ketamine can help rescue the young soccer players trapped in a flooded Thailand Cave (literally one of the most austere environments ever described), then I am positive it can help alleviate the anxiety and pain encountered within my ED. We have discussed using ketamine in various situations in the past (ex, Post-Tonsillectomy Hemorrhage, Delayed Sequence Intubation), but it is most often used for pain management or procedural sedation (ex, Incision and Drainage). Since it is used commonly, we may become a bit too comfortable with it … and forget that ketamine can have adverse events (because nothing is perfect). Let’s make sure that we remember some of the most Severe Adverse Events associated with Ketamine and know what to do when Ketamine and Laryngospasm commingle in the some room:
Ketamine: Why We (I) Love It!
- Quick Onset
- No Respiratory Depression
- Analgesic and Dissociative
- Requires little monitoring
- again… see the Thailand Cave Rescue story — no monitoring there and they were using SCUBA.
- Clearly, always follow your hospital’s protocols.
- Has been found to be Safe and Effective [Grunwell, 2016; Green, 2010]
- Used for a W I D E range of applications
- From Austere and (literal) War Zones to the very controlled Operating Room
- Many examples of utility in the Emergency Department.
- Actually listed on the WHO list of Essential Medications.
Ketamine: Severe Adverse Events
Ok, so we love Ketamine and often consider it to be nearly perfect… but it is not without its potential problems. We all are aware of the more common and, relatively minor, side effects like nausea/vomiting, but let’s focus on the Severe Adverse Events. [Grunwell, 2016; Green, 2010]
- Severe Adverse Events that have been described with Ketamine administration:
- Airway Obstruction (resolves with repositioning)
- Laryngospasm (not relieved with repositioning)
- Requiring Emergent Airway Intervention (ex, Positive Pressure Ventilation, Supraglottic Airway, Intubation)
- Aspiration
- Cardiac Arrest
- Severe Adverse Events related to Ketamine administration are, fortunately, rare.
- A large prospectively collected database of pediatric ketamine sedations OUTSIDE the OR found: [Grunwell, 2016]
- All types of Adverse Events were reported in 7.3% of cases.
- Severe Adverse Events were reported in 1.77% of cases.
- Risk Factors for: [Grunwell, 2016; Green, 2010]
- Patients with cardiac or gastrointestinal disorders
- Patients with lower respiratory tract infections
- Co-administration with Propofol
- Co-administration with Anticholinergics
- Anticholinergics, historically, were advocated to be used to help prevent complications by decreasing secretions and cough (which were thought to increase risk for laryngospasm)…. BUT…
- Now atropine or glycopyrrolate are now longer recommended to be used reflexively as they do not decrease risk. [Grunwell, 2016; Green, 2010]
Ketamine and Laryngospasm
Basics
- The incidence of laryngospasm as a Severe Adverse Event related to ketamine is very low (~0.3%), but still occurs.
- It is not easily predicted and appears to be idiosyncratic. [Green, 2010]
- Anticholinergics do not reduce its risk of occurring. [Grunwell, 2016; Green, 2010]
- Providers must be prepared for it!
Treatment
- Step 1: Be prepared for the worst (like always)
- Prepare resuscitation bag-valve mask and have it ready.
- Have advanced airway equipment in room (within reach ideally).
- Use End-tidal CO2 monitoring.
- Step 2: Open the Airway (basics are best)
- The airway may be obstructed, but you may not be encountering actual laryngospasm.
- Align and open the airway… anticipating the challenges inherent in children’s airways.
- If not laryngospasm, optimizing position will likely correct the problem.
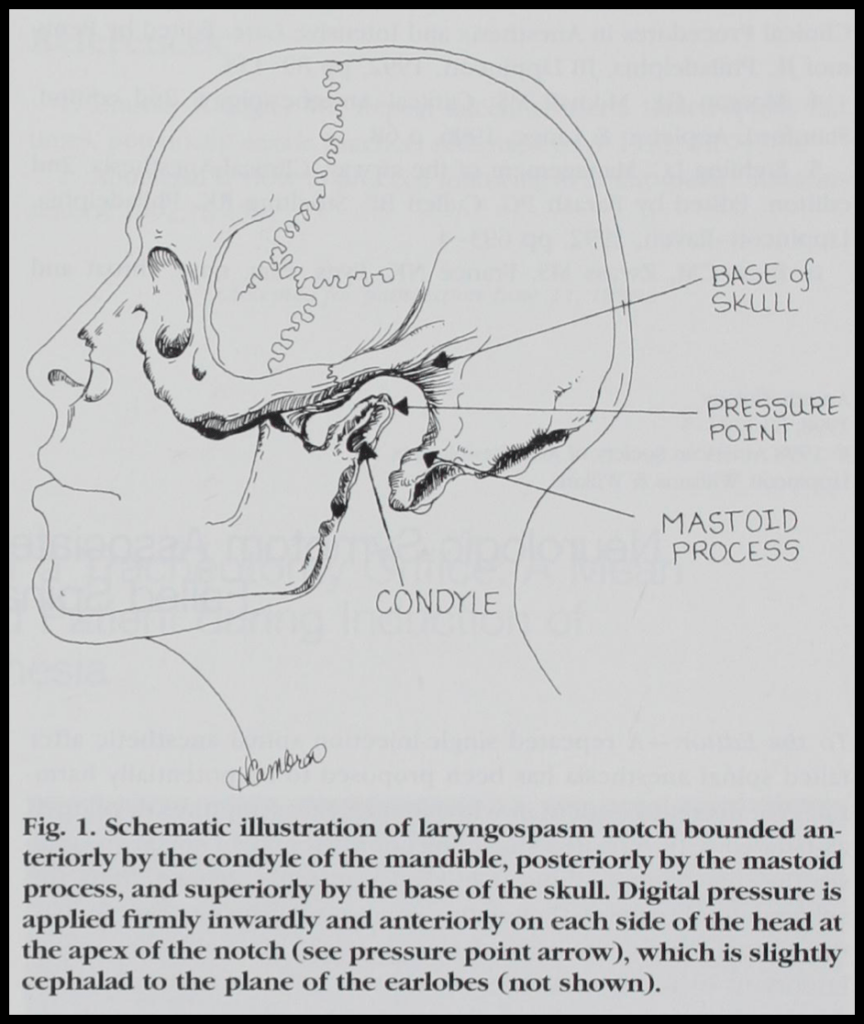
- Step 3: Apply Pressure to the “Laryngospam Notch” [Larson, 1998]
- So, I was taught this… and never knew where it “came from”… seems like it comes from Dr. Larson who learned it from Dr. Guadagni. I have asked our beloved Anesthesiologist (Dr. Blasius) and have confirmation that this is still taught (so I am not that old).
- The “Laryngospasm Notch”:
- Behind the earlobe and the Mandible’s Ramus
- In front of the mastoid process
- PUSH HARD Medially (toward the skull base) and Anteriorly (like a jaw thrust – but much meaner)
- May avoid needing any additional therapy… but have someone getting the BVM and airway equipment now…
- Step 4: Positive Pressure Ventilation
- If the laryngospasm has not yet resolved, then it is time to use some Positive Pressure Ventilation.
- The combination of “Laryngospasm Notch” pressure and PPV may resolve issue… but…
- Step 5: RSI
- Ideally we have avoided needing this step… but… this is why were are always prepared and slightly paranoid.
Moral of the Morsel
- It may be very rare, but expect it to happen to you. Being paranoid is not a bad thing when sedating people.
- Being a little bit mean may help someone breath. Push on the “Laryngospasm Notch” with the intent to make the patient breath.
- Sometimes paralytics are required. If those laryngeal muscles won’t cooperate… make them go to sleep too.

