Pediatric Sinus Bradycardia
Pediatric cardiac issues can make even the most experienced EM MD have axillary perspiration more than normal. We have covered many cardiac entities in the Morsels (Hypercyanotic Spells, Heart Failure, HTN, Coaractation, Fontan Complications, PGE1, Syncope, and Kawasaki Disease) as these are conditions that are not encountered everyday and, therefore, it is good to remind ourselves of them so we don’t get too sweaty when dealing with them. We are likely more comfortable with arryhthmias than structural heart disease. SVT can even be fun to manage. The question I have is, what am I supposed to do with asymptomatic SINUS BRADYCARDIA? Do I need to get sweaty and nervous and can I be mellow and cool?
Arrhythmias in Kids
- Arrhythmias due to a primary cardiac condition are rare in kids in the pediatric ED.
- Arrhythmias are rarely the initial presentation of structural heart disease in children.
- Most children with structural heart disease will present with signs of heart failure or cyanosis.
- One study showed that only 7% of pediatric cardiology patients had a primary arrhythmia.
- Incidence of arrhythmia in the Ped ED has a BiModal distribution.
- Infancy
- Most infant tachyarrhythmias resolve within 1st year of life
- Adolescence
- Heart size increases – thought to increase risk of developing re-entrant pathways.
- Older kids are also able to describe symptoms better.
- Higher likelihood of medication or illicit substance related arrhythmias.
- Infancy
Sinus Bradycardia
- Sinus Bradycardia is almost never due to a primary cardiac issue in children.
- Defined as:
- < 100 bpm in kids 0-3 years old
- < 60 bpm in kids 3-9 years old
- < 50 bpm in kids 9-16 years old
- Kids with benign sinus bradycardia are asymptomatic and have benign clinical courses.
Sinus Bradycardia Evaluation
- Dont’ get ahead our yourself… is this Sinus? Remember “Worst First“.
- Is the patient hemodynamically stable? If not, fix the problem!
- Look closely for evidence of AV-Blocks (1st, 2nd, 3rd degree?).
- Consider “sick sinus syndrome”
- An irregular tachycardia followed by a slowed SA node discharge.
- Will have a failure of HR to increase in response to exercise or stress.
- Usually seen in kids s/p operative repair of congenital heart disease.
- Ask yourself, “Why?”
- Since Sinus Bradycardia is generally not a primary cardiac etiology, so it’d be good to consider other causes.
- Consider the follow:
- Things we often think of, but generally are obvious (the H’s and T’s):
- Hypoxia
- Heart Block
- H+ ions
- Hypothermia
- Hyperkalemia/Hypokalemia
- Trauma (Increased ICP)
- Toxins (Lithium, digoxin, Beta-blockers, Ca-Channel Blockers, Clonidine)
- Things to not under-appreciate (also known as things that I need to remember, cuz I keep forgetting them):
- Hypoglycemia
- Hypothyroidism
- Malnutrition
- Anorexia Nervosa
- Things we often think of, but generally are obvious (the H’s and T’s):
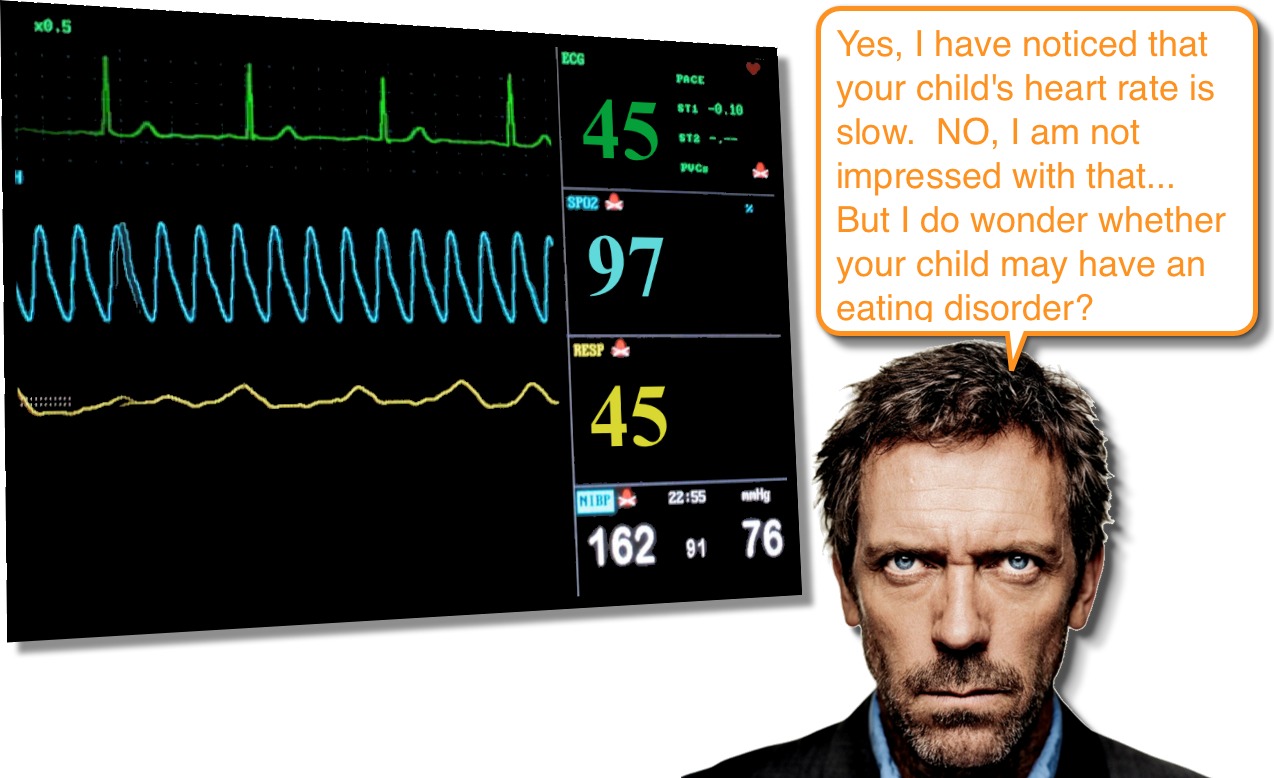
So, while the overall clinical course of Pediatric Sinus Bradycardia is benign and reassuring, take the opportunity to consider other entities, particularly eating disorders. Many times the child with sinus bradycardia is athletic and we are eager to attribute the sinus bradycardia to the athletic conditioning; however, recall that eating disorders can also be associated with athletes … both males and females!!
References
Chiu SN, Lin LY, Wang JK, Lu CW, Chang CW, Lin MT, Hua YC, Lue HC, Wu MH. Long-term outcomes of pediatric sinus bradycardia. J Pediatr. 2013 Sep;163(3):885-9. PMID: 23623512. [PubMed] [Read by QxMD]
Egan KR, Ralphe JC, Weinhaus L, Maginot KR. Just sinus bradycardia or something more serious? Case Rep Pediatr. 2013;2013:736164. PMID: 23476865. [PubMed] [Read by QxMD]
Doniger SJ, Sharieff GQ. Pediatric dysrhythmias. Pediatr Clin North Am. 2006 Feb;53(1):85-105, vi. PMID: 16487786. [PubMed] [Read by QxMD]
Sacchetti A, Moyer V, Baricella R, Cameron J, Moakes ME. Primary cardiac arrhythmias in children. Pediatr Emerg Care. 1999 Apr;15(2):95-8. PMID: 10220076. [PubMed] [Read by QxMD]


e my 7years old boy accidently find out with missed pulse and HR 62bpm.But it raises during activity .Seen by pediatric cardiologist done Complete ECHO,ECG ,and Holter for 24 Hrs. all is normal holter test result still pending. .He is asyptomatic. His elder sister was having ASD and it closed through Open heart surgery .So I am more concerned about his issue. usually bradycardia due to what reason,and what is the normal holter result pls advise
Our eight year old daughter was recently diagnosed with a 20% tricuspid insufficiency and we were told that is the source of her chest pain but to not worry about it as it’s not big deal. The chest pain, in and of itself, is a concern and an issue though. Her pain is so frequent and so severe that it wakes her multiple times a night, prevents her from participating in sport and has resulted in her being sent home from school three times in two weeks. Add to this she has an irregular heart rate (anywhere from 42 to 137 bpm) and we were just told she now shows a sinus arrhythmia, which did not show on the ecg done three weeks ago (that one was completely normal while now she shows the arrhythmia along with a prolonged QTc). I know you cannot give specific medical advice but would you recommend we seek a second opinion or trust the cardiologist who says it’s all of no concern and our daughter should just change position when she is in pain. He says he will see her again in one year.
I am sorry that you are dealing with this. I know it can be distressing to have a child who isn’t feeling well.
It is always advisable to first discuss continued symptoms with your original providers. Often what is recommended is for what would be expected for the majority of cases, but there are always secondary (or “backup”) plans that can be put into play if necessary. I think open communication about patients’ and families’ concerns is important to ensure everyone is on the same page. Involving “second opinions” before the first has really played out all of the possibilities can often lead to an equal amount of frustration.
So, while I cannot give specific advice to you, I hope what I have said is helpful.
-sean
Just researching and came across this article – My son just turned 10. He was diagnosed with PANS/PANDAS in April 2019, but his symptoms started in October 2018. Lots of doctor visits since last October when we began to pay attention to his heart rate. Resting heart rate is typically in upper 50’s to low 60’s. Last week, he had his tonsils/adenoids removed due to the repeated strep and a history of rheumatic fever in the family. The anesthesiologist was concerned with about his heart rate which hung around 50 after surgery, even dropping to the low 40’s. He was an active, healthy kid before all of this started in October. We don’t have a good baseline of before October except for doctor appts. in which it appeared to be mostly in the low 80’s. He had an in-office EKG at one of his doctor’s appts and all appeared to be ok. His pediatrician checked him out and said she thinks he’s just athletic. Do I pursue this with a specialist?
My 14 year old son has moderat left side hydronephrosis from birth due to extra renal pelvis asymptomatic. Not on any treatment. Recently noticed his heart rate 45 to 50 .echo done it’s normal. Is there any other test to diagnose? Pls advise.
Ms. Jacob, I cannot give out specific, individual medical advice out over the internet. I would recommend that you address your concerns and questions with your son’s physicians. I am certain that they will help guide you.
All the best!
Thank you,
sean
How many people a year suffer from bradycardia in America?
My 16 year old son was diagnosed with sinus bradycardia and he is not atheletic at all and has never been on medications other than some antibiotics and. Does this mean he either he has a heart blockage or his natural pacemaker is not working and will probably in the end need a pacemaker put in
Juanica,
I am, naturally, unable to give out medical advice over the internet, so would encourage you to discuss these concerns with your child’s primary care doctor. I will say that this can be a normal finding in a lot of children.
Thank you,
sean
Hi I was reading about your son’s issues do you mind to share what you found out from your physical my son has same problems as well and Dr can’t find out what is wrong to give a diagnosis.
I am a nurse/paramedic. My son was recently seen for a sinus infection at our PCP office by one of his NP’s. My son’s heart rate was 50. He was asymptomatic. He recently complained of a dizzy spell after running for some distance in gym class which resolved quickly with rest. My son never sits. He plays several sports many of them overlap. He has never had any sign or symptom during any of these sporting events like he did that day at school. Other than checking his pulse and recording it for several days at interval times is there anything else we should be doing. I am cautiously concerned but his Mother is ready for a cardiology consult. Any thoughts.
Obviously, I am unable to give any specific medical advice out over the Internet, but I would say that it sounds like you are doing a great job and discuss this further with his primary care doctor (and perhaps get an ECG).
Thank you, sean
how and what can you do to treat a bradycardia in a teen with a eating disorder ?
Sam,
Generally, it is just supportive… their bradycardia does not typically lead to hemodynamic instability, unless there is significant electrolyte derangements. Therapy should be directed toward correcting those derangements (although do so carefully).
Thank you,
sean
[…] population that requires special consideration of the differences in anatomy and physiology (ex, Sinus Bradycardia, Aortic Trauma, Back Pain, Traumatic Pneumothorax). What is equally important to remember is that […]
[…] are less dramatic. Patients with Eating Disorders can often present with subtle cues (see Bradycardia) and if you are vigilant, you can make a profound difference — just like you always wanted to […]
[…] Sinus bradycardia is probably the most common thing in paeds that we are asked to review on the ward, and a frequent (incidental) finding in ED. Sean Fox writes a great morsel on this at PED EM Morsels. [TRD] […]
Thank you!