Pneumomediastinum
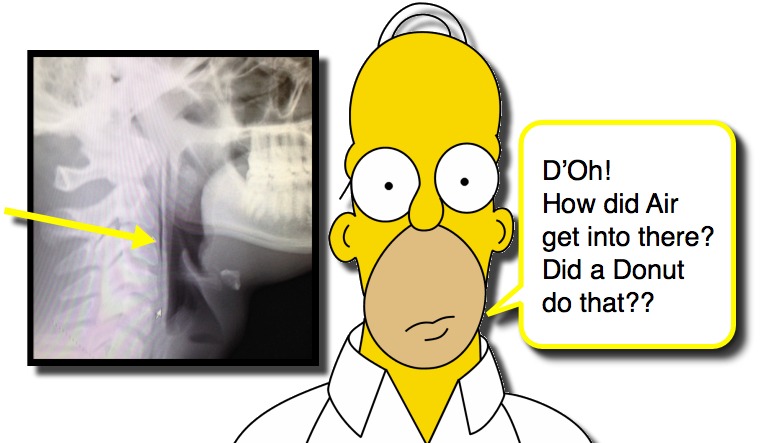
Every so often you encounter a patient that has a finding that catches you by surprise. Like having air in places that should not have air in them. We have discussed spontaneous pneumothorax and traumatic pneumothorax in children as well as how to detect pneumothorax in neonates and how to treat a pneumothorax, but what about pneumomediastinum? As you try to resist the urge to say “D’Oh!” let us consider Pneumomediastinum!
Pneumomediastinum Basics
- Symptoms
- Pain – Chest Pain, Neck Pain, Throat Pain
- Hoarseness, Stridor, Cough
- Globus Pharyngeus – persistent or intermittent, non-painful sensation of swelling or foreign body in throat.
- Dyspnea, Choking
- Facial and/or Neck Swelling
- Imaging Modality
- Lateral Neck Soft Tissue plain film is more sensitive than PA CXR (95.2% vs 89.1%). (Wang, 2013)
- CT is certainly more sensitive than plain radiographs, but would not be a reasonable screening strategy.
Pneumomediastinum Causes
- Primary Pneumomediastinum = presence of air within the mediastinum with NO obvious precipitating event.
- Of cases of pneumomediastinum one study found ~50% were Spontaneous Primary Pneumomediastinum. (Wong, 2013)
- Secondary Pneumomediastinum = Pneumomediastinum is present due to a defined etiology:
- Spontaneous (Wong, 2013)
- Asthma Exacerbation – ~17%
- Pneumonia or Lower Respiratory Tract Infection – ~13%
- Choking Events / Foreign Body Aspiration – ~12%
- Viral Illness / Cough / Croup – ~3%
- Spontaneous esophageal or bronchial rupture are very rare causes of pneumomediastinum in kids.
- Traumatic (Pryor, 2011)
- Relatively uncommon after trauma to neck, thorax, or abdomen.
- Can be associated with life-threatening tracheobronchial, esophageal, or vascular injuries.
- All of the patients who had significant injury to trachea/bronchus, esophagus, or vascular structures were identified on CXR.
- Most common associated injuries found with complicated pneumomediastinum were:
- Pneumothorax
- Rib Fractures
- Lung Contusion
- Hemothorax
- Less common to see significant mediastinal injuries in children than adults.
- Spontaneous (Wong, 2013)
Age Matters with Pneumomediastinum
- In children less than 6 years of age, spontaneous primary pneumomediastinum is very rare. (Wang, 2013)
- For young kids, look more diligently for a cause of the pneumomediastinum.
- Asthma exacerbation is a common cause.
- Keep Foreign Bodies on the DDx as they can be tricky. (Hu, 2012)
- With a history of choking / gagging, have a low threshold to obtain bronchoscopy / esophagoscopy.
- Children older than 6 can have spontaneous primary pneumomedisastinum.
- Base evaluation of it on the history and presentation.
Advanced Investigations??
- Naturally, the question is what needs to be done once you have diagnosed the pneumomediastinum.
- When do you need to look for potential causes of Secondary Pneumomediastinum?
- Here is a proposed strategy (Wang, 2013):
- Manage conservatively if:
- Presents with an asthma exacerbation,
- Presents with recent onset of fever,
- Presents with vigorous cough,
- Presents with NO choking episodes.
- Consider further investigations as indicated (ex, bronchoscopy, esophagoscopy, Upper GI/Swallow study, Chest CT) if:
- Presents after a catastrophic event,
- Presents after a choking episode,
- Presents with dysfunctional swallowing,
- Presents after trauma and has clinical evidence of aerodigestive injury. (Neal, 2009)
- Consider Age
- Have lower threshold for further evaluation in the younger child (as they are less likely to have spontaneous primary pneumomediastinum.
- Extensive diagnostic evaluations in uncomplicated spontaneous pneumomediastinum in adolescents is often unnecessary.
- Consider Clinical Course
- Kids with isolated pneumomediastinum, no other abnormalities on CXR, and low risk mechanism (if traumatic) are at at low risk for tracheobronchial, esophageal, or vascular injuries, so observation alone would be appropriate; however, if clinically worsens, than reconsider other potential problems. (Pryor, 2011)
- Not all that wheezes is asthma… Foreign Bodies can be difficult to diagnose, so reconsider this potential if patient does not respond to therapy as you’d expect.
- Manage conservatively if:
References
Wong KS1, Wu HM, Lai SH, Chiu CY. Spontaneous pneumomediastinum: analysis of 87 pediatric patients. Pediatr Emerg Care. 2013 Sep;29(9):988-91. PMID: 23974718. [PubMed] [Read by QxMD]
Hu M1, Green R, Gungor A. Pneumomediastinum and subcutaneous emphysema from bronchial foreign body aspiration. Am J Otolaryngol. 2013 Jan-Feb;34(1):85-8. PMID: 23102886. [PubMed] [Read by QxMD]
Pryor SD1, Lee LK. Clinical outcomes and diagnostic imaging of pediatric patients with pneumomediastinum secondary to blunt trauma to the chest. J Trauma. 2011 Oct;71(4):904-8. PMID: 21460747. [PubMed] [Read by QxMD]
Neal MD1, Sippey M, Gaines BA, Hackam DJ. Presence of pneumomediastinum after blunt trauma in children: what does it really mean? J Pediatr Surg. 2009 Jul;44(7):1322-7. PMID: 19573655. [PubMed] [Read by QxMD]


[…] and complications. Previously, we have discussed abnormal collections of air (ex, pneumothorax, pneumomediastinum). Now, let us look at another potentially alarming situation- Pneumatosis […]
[…] We have discussed several causes of chest pain in the past (ex, myocarditis, pulmonary embolism, pneumomediastinum, spontaneous pneumothorax), but one that deserves some attention now is […]
Good post. I learn something new and challenging on sites I stumbleupon everyday.
It’s always helpful to read content from other authors and use a little something from their websites.