Uveitis
Uveitis: Basics
- Uveitis is a rare, but significant disorder.
- 3rd leading cause of blindness in developed countries.
- Complications are frequent. [Sardar, 2017]
- Retinopathy
- Cataract
- Blindness (accounts for ~20% of pediatric blindness)
- Uveitis more commonly affects adults, but:
- The posterior chamber of the eye is more likely to be involved in kids and,
- Children are more likely to develop blindness from it.
- Causes of uveitis include:
- Idiopathic – occurs without associated systemic illness in 30-50% of cases
- Juvenile Idiopathic Arthritis (JIA) is the leading defined cause
- Uveitis is the most common extra-articular manifestation of JIA.
- 10-20% of patients with JIA are at risk for uveitis.
- Young age at onset of arthritis (< 7 years), +ANA, +antihistone antibodies, and oligoarticular JIA were risk factors for development of uveitis. [Nordal, 2017]
- Majority of uveitis cases develop within first 4 years of JIA diagnosis.
- Behcet Disease
- Sarcoidosis
- Lupus
- Inflammatory Bowel Disease
- Infections
- Syphilis
- Chlamydia
- HIV/AIDS
- Tuberculosis
Uveitis: Presentation
- Presentations is varied.
- Can present with acute symptoms, but
- Can also be insidious and be asymptomatic.
- Symptoms related to compartment involved:
- Anterior
- Eye Pain and Photophobia
- Red Eye
- Posterior
- Blurred vision and floaters
- Can by asymptomatic
- Anterior
- Can also find:
- Increased Intraocular Pressure [Kothari, 2015]
- Vision Loss – ~25% will be legally blind
- Risk factors for severe uveitis (sight-threatening): [Angeles-Han, 2016]
- Short duration between development of arthritis and uveitis
- Young age at uveitis onset
- Uveitis diagnosed before arthritis
- Male gender
Uveitis: Therapy
- Corticosteroids
- Typically used as first line.
- Topical or systemic therapies have been used.
- Immunomodulator Drugs
- Methotrexate and azathioprine are second-line therapies.
- Mycophenolate mofetil as also been used.
- Anti-TNF-alpha monoclonal antibodies are effective. [Sardar, 2017]
- Even with appropriate therapy, cases are often recurrent.
- Conventional therapies are often insufficient. [Sardar, 2017]
- Chronic, remittent course is common and many will require long-term therapy. [Angeles-Han, 2016]
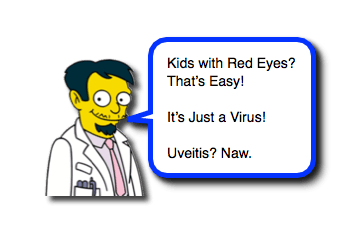
Moral of the Morsel
- Be vigilant! Not all red eyes are due to viruses.
- Ask the right questions. History of rheumatologic problems in patient or strong family history of them… consider uveitis.
References
Nordal E1, Rypdal V2, Christoffersen T3, Aalto K4, Berntson L5, Fasth A6, Herlin T7, Nielsen S8, Peltoniemi S4, Straume B9, Zak M8, Rygg M10; Nordic Study Group of Pediatric Rheumatology (NoSPeR). Incidence and predictors of Uveitis in juvenile idiopathic arthritis in a Nordic long-term cohort study. Pediatr Rheumatol Online J. 2017 Aug 18;15(1):66. PMID: 28821293. [PubMed] [Read by QxMD]
Sardar E1, Dusser P2, Rousseau A3, Bodaghi B4, Labetoulle M3, Koné-Paut I2. Retrospective Study Evaluating Treatment Decisions and Outcomes of Childhood Uveitis Not Associated with Juvenile Idiopathic Arthritis. J Pediatr. 2017 Jul;186:131-137. PMID: 28457525. [PubMed] [Read by QxMD]
Angeles-Han ST1, Rabinovich CE. Uveitis in children. Curr Opin Rheumatol. 2016 Sep;28(5):544-9. PMID: 27328333. [PubMed] [Read by QxMD]
Hettinga YM1, de Groot-Mijnes JD2, Rothova A3, de Boer JH1. Infectious involvement in a tertiary center pediatric uveitis cohort. Br J Ophthalmol. 2015 Jan;99(1):103-7. PMID: 25138763. [PubMed] [Read by QxMD]
Kothari S1, Foster CS2, Pistilli M3, Liesegang TL4, Daniel E5, Sen HN6, Suhler EB7, Thorne JE8, Jabs DA9, Levy-Clarke GA10, Nussenblatt RB6, Rosenbaum JT11, Lawrence SD12, Kempen JH13; Systemic Immunosuppressive Therapy for Eye Diseases Research Group. The Risk of Intraocular Pressure Elevation in Pediatric Noninfectious Uveitis. Ophthalmology. 2015 Oct;122(10):1987-2001. PMID: 26233626. [PubMed] [Read by QxMD]


Managing uveitis will always be challenging. It will always benefit from informed guidance from rheumatologists and uveitis specialists, but I am excited about the new technologies that will ease the challenge of drug delivery for both patients and physicians in the coming years.