Discitis and Spondylodiscitis in Children
We all know that caring for children can be tricky. Being a parent is certainly tricky… but trying to decipher the subtle clues a child presents with to ensure that nothing ominous is lurking underneath the non-specific complaints is unquestionably challenging! Does that fever warrant concern for entities on the Ddx list of Fever of Unknown Origin? We often look for “Red Flags” to help us navigate the morass, but red flags can also be misleading when we have to consider adults as well as children. Consider “Back Pain” complaints. In adults, we look for the “red flags” and when they are not present, we feel rather confident that it is a benign, self-limited condition. Is the same true for children? Sadly, no. Back Pain in children warrants concern. Let’s take a moment to digest a Morsel on one potential cause of Pediatric Back Pain – Discitis in Children:
Discitis in Children: Basics
- Discitis = infection in the vertebral disc. [Fernandez, 2000;Principi, 2016]
- It is often accompanied by infection in the adjacent vertebral body (i.e., spondylodiscitis)
- Most believe that the conditions exist on a spectrum from discitis to spondylodiscitis to vertebral osteomyelitis.
- 3 peak pediatric age groups [Fernandez, 2000;Principi, 2016]
- Neonatal – few months of age (may be irritable or septic)
- 6 months of age – preschool age (may have nonspecific limp)
- School-aged and adolescence (may have complaint of back pain)
- Infectious Discitis can be classified as: [Fernandez, 2000; Principi, 2016]
- Pyogenic
- Most common form (~90% of cases)
- Most cause = Staph Aureus (~80% of cases)
- Kingella kingae – SIGNIFICANT PATHOGEN in children 6 months – 4 years! [Fernandes Machado, 2017]
- Others = Coag-neg Staph, Strep pneumoniae, Gram-neg rods, E. Coli, Salmonella spp.
- Actually obtaining positive cultures is difficult.
- Specific
- example: Tuberculosis
- Frequency depends on geographic region.
- ~5% of all extra pulmonary tuberculosis cases involve bones and joints and the spine is the most common site.
- example: Brucella spp.
- Unpasteurized goat cheese consumption history.
- Creates subacute and chronic presentation.
- example: Tuberculosis
- Unspecific Granulomatous
- Parasitic
- Pyogenic
- Infectious Discitis (and spondylodiscitis) occur due to: [Principi, 2016]
- Hematogenous spread (primarily)
- Direct inoculation and local extension
- Surgical procedures or local trauma
- Several cases related to complication of ingestion of Button Batteries.
Discitis in Children: Anatomy Matters
- Vertebral discs are vascularized during early childhood. [Principi, 2016]
- Blood vessels are present in the cartilaginous vertebral endplate until ~ 7 years of age.
- Blood vessels can be present in the annulus fibrosis until up to 20 years of age.
- Presence of blood vessels allows hematogenous spread.
- Spongy bone is supplied by end arteries in older children and adolescents. [Principi, 2016]
- Transient bacteremia can lead to small infectious emboli becoming lodged in the bone and then proliferate.
- Infection can spread, then, from the bone to the disc.
- In children the infection may begin first in the disc and then spread to the adjacent structures and bone or vice versa. [Fernandez, 2000;Principi, 2016]
- Younger children more commonly develop discitis first.
- Older children more commonly develop vertebral osteomyelitis first.
Discitis in Children: Evaluation & Management
- Presentation: [Fernandez, 2000;Principi, 2016]
- Presentation will vary based on age.
- Neonates and young infants may present with sepsis or irritability.
- Toddlers and young children:
- Back Pain
- Refusal to ambulate
- Limping (Ddx list of SCFE, Toddler’s Fx, and Septic Arthritis)
- Need for support while standing
- Pain with flexing thighs
- Low-grade fever (although not common)
- RARELY will have neurologic symptoms or complaints
- Older children (who are more likely to have spondylodiscitis and/or osteomyelitis) often have more systemic symptoms.
- Fever
- Back pain
- Ill-appearance
- Location matters:
- Lumbar involvement is more common and can affect ambulation / gait.
- Cervical involvement can lead to torticollis or dysphagia. [Scheuerman, 2015]
- Early symptoms and findings are nonspecific.
- Delays in diagnosis are common (often delays of 4-6 months).
- Early diagnosis is, however, beneficial to avoid complications.
- Presentation will vary based on age.
- Evaluation: [Fernandez, 2000;Principi, 2016]
- Lab values are often not useful.
- Inflammatory markers may be elevated, but lack of abnormal labs does not rule out the condition.
- Do obtain Blood Cultures… may help improve determining the pathogen.
- Serology can be helpful also (ex, Cat Scratch history? B. henselae infection can cause vertebral osteomyelitis. Check serologic testing)
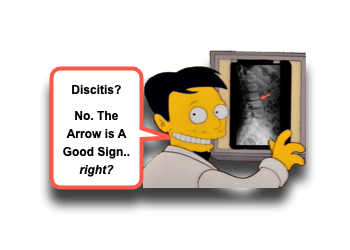
- Imaging:
- Plain radiographs may show abnormalities, but usually not until after 2-6 weeks of illness.
- MRI is the preferred imaging modality at this point (~96% sensitive).
- MRI helps with both the diagnosis and determination of whether surgical management is required.
- Lab values are often not useful.
- Treatment: [Fernandez, 2000;Principi, 2016]
- Information about the offending pathogen is important, but difficult to obtain.
- Fine needle aspiration or traditional biopsy are often used to obtain samples.
- Some recommend not giving empiric antibiotics to patients until cultures obtained.
- In the systemically ill appearing child, personally, I would not delay antibiotics… but fortunately most often the patient is not systemically ill.
- Antibiotics often given intravenously for ~2 weeks and then orally for several weeks following.
- Bedrest – Allows for healing to occur and can maintain spine in normal anatomic position.
- Surgical interventions – required for failure of conservative therapy, vertebral compression or destruction, or intractable pain.
- Information about the offending pathogen is important, but difficult to obtain.
Moral of the Morsel
- Don’t just prescribe ibuprofen. Back Pain in children warrants more consideration.
- Infections can happen without Fever. Don’t eliminate your concern for discitis merely due to the lack of a fever.
- Limping isn’t just a leg thang! If you thought you were going to find a cause of the limp on those leg x-rays and didn’t… consider looking higher.
- Anticipatory Guidance!! Not everyone needs an MRI… but everyone needs good anticipatory guidance. Persistent symptoms require reconsideration!

