Group B Strep (GBS): Early, Late, and Very Late
Group B Strep: Basics
- Group B Strep is a significant cause of invasive bacterial infections (ex, meningitis and sepsis) in neonates and infants less than 3 months.
- Due to newborn becoming colonized by maternal flora.
- ~20-25% of pregnant women are colonized by GBS. [Oh, 2013]
- Factors associated with higher risk for transmission of GBS: [Oh, 2013]
- Previous Sibling with GBS Disease
- Prematurity (<37 weeks GA)
- Prolonged Rupture of Amniotic Membranes
- Maternal GBS UTI during pregnancy
- Maternal Fever
- Screening programs and intrapartum antibiotics have successfully reduced the incidence of Early Onset GBS, but not Late Onset GBS.
Group B Strep: Timing is Everything
- Early Onset GBS
- Occurs in neonates in first week (< 7 days) of life.
- Typically present with symptoms in the first 48 hours and likely caught before hospital discharge; however,:
- Can develop symptoms after discharge or
- Can develop subtle symptoms that go unnoticed prior to discharge… so…
- The patient may be presenting to your ED!
- Has two presentation forms[Oh, 2013]:
- Acute Respiratory Distress
- Develops very soon after birth.
- Appears clinically ill.
- Due to direct pulmonary capillary injury and pulmonary edema.
- Can progress to pulmonary hypertension and cardiovascular collapses as well as DIC.
- Rarely has concurrent meningitis.
- Sepsis Presentation
- Seen in infant born to an untreated / inadequately treated mother colonized by GBS.
- Initially appeared well at birth, but then develops:
- Apnea
- Cyanosis
- Poor feeding
- Hypo/hyperthermia
- Lethargy
- Evolves into overt sepsis.
- Higher risk for meningitis.
- Acute Respiratory Distress
- Late Onset GBS
- Occurs in infants 7-89 days of life.
- Intrapartum screening and antibiotic programs have NOT reduced incidence.
- Likely has different risk factors and routes of transmission. [Bartlett, 2017]
- May not be from exposure during delivery, but other maternal contact. [Bartlett, 2017]
- Typical Risk Factors of Early Onset GBS are not prevalent in Late Onset GBS patients. [Bartlett, 2017]
- Noted to have higher morbidity and mortality than Very Late Onset GBS. [Bartlett, 2017]
- Can have concurrent meningitis, which is associated with worse outcomes. [Bartlett, 2017]
- Patients with GBS meningitis are more prone to develop seizures, abnormal neuroimaging (ex, infarcts), and abnormal neuro-development. [Bartlett, 2017]
- Very Late Onset GBS
- Occurs in infants and children >90 days of life.
- Intrapartum screening and antibiotic programs have NOT reduced incidence.
- Has similar patient presentations as Late Onset GBS. [Bartlett, 2017]
- Late Onset and Very Late Onset GBS Presentations
- Presentations can be very subtle at first… and then, may become dramatic.
- Vigilance is required on our part.
- May have:
- Marked irritability, inconsolability, high-pitched cry
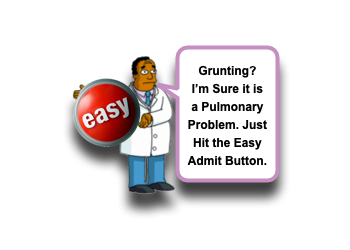
- Constant GRUNTING
- Grunting is never good.
- Don’t be deceived into thinking that the grunting points specifically to a pulmonary etiology. Keep Ddx open!
- Apnea and abnormal breathing
- Prolific / projectile vomiting (particularly if bilious)
- Poor Feeding
- Poor Perfusion
- Poor Tone / Floppy
- Bulging Fontanelle
Moral of the Morsel
- Grunting is Never Good! Ok… that was Easy.
- Grunting Does NOT = Pulmonary Cause! That is the hard part. Keeping serious bacterial infections as a potential etiology of grunting can be challenging, particularly during Bronchiolitis Seasons.
- GBS Does Not only infect neonates! Late Onset GBS and Very Late Onset GBS can occur past the 1st month of life.
References
Coon ER1,2, Srivastava R3,2,4, Stoddard G2,5, Wilkes J4, Pavia AT2,6, Shah SS7,8. Shortened IV Antibiotic Course for Uncomplicated, Late-Onset Group B Streptococcal Bacteremia. Pediatrics. 2018 Nov;142(5). PMID: 30309887. [PubMed] [Read by QxMD]
Bartlett AW1, Smith B, George CR, McMullan B, Kesson A, Lahra MM, Palasanthiran P. Epidemiology of Late and Very Late Onset Group B Streptococcal Disease: Fifteen-Year Experience From Two Australian Tertiary Pediatric Facilities. Pediatr Infect Dis J. 2017 Jan;36(1):20-24. PMID: 27749655. [PubMed] [Read by QxMD]
Giannoni E1, Berger C, Stocker M, Agyeman P, Posfay-Barbe KM, Heininger U, Konetzny G, Niederer-Loher A, Kahlert C, Donas A, Leone A, Hasters P, Relly C, Baer W, Aebi C, Schlapbach LJ; Swiss Pediatric Sepsis Study Group. Incidence and Outcome of Group B Streptococcal Sepsis in Infants in Switzerland. Pediatr Infect Dis J. 2016 Feb;35(2):222-4. PMID: 26535881. [PubMed] [Read by QxMD]
Oh W1. Early onset neonatal group B streptococcal sepsis. Am J Perinatol. 2013 Feb;30(2):143-7. PMID: 23322392. [PubMed] [Read by QxMD]
Verani JR1, McGee L, Schrag SJ; Division of Bacterial Diseases, National Center for Immunization and Respiratory Diseases, Centers for Disease Control and Prevention (CDC). Prevention of perinatal group B streptococcal disease–revised guidelines from CDC, 2010. MMWR Recomm Rep. 2010 Nov 19;59(RR-10):1-36. PMID: 21088663. [PubMed] [Read by QxMD]
Centers for Disease Control and Prevention (CDC). Trends in perinatal group B streptococcal disease – United States, 2000-2006. MMWR Morb Mortal Wkly Rep. 2009 Feb 13;58(5):109-12. PMID: 19214159. [PubMed] [Read by QxMD]
Baltimore RS1. Consequences of prophylaxis for group B streptococcal infections of the neonate. Semin Perinatol. 2007 Feb;31(1):33-8. PMID: 17317425. [PubMed] [Read by QxMD]
Centers for Disease Control and Prevention (CDC). Perinatal group B streptococcal disease after universal screening recommendations–United States, 2003-2005. MMWR Morb Mortal Wkly Rep. 2007 Jul 20;56(28):701-5. PMID: 17637595. [PubMed] [Read by QxMD]
Centers for Disease Control and Prevention (CDC). Early-onset and late-onset neonatal group B streptococcal disease–United States, 1996-2004. MMWR Morb Mortal Wkly Rep. 2005 Dec 2;54(47):1205-8. PMID: 16319814. [PubMed] [Read by QxMD]


[…] Neonatal Group B strep infections over at Ped EM Morsels […]