Penicillin for Pneumonia
Infectious diseases are commonly considered when dealing with pediatric patients. We have covered topics in this realm numerous times (I believe that this would be the 64th Morsel in the ID category). One of the more prevalent considerations is pediatric pneumonia.
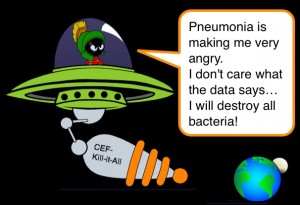
Previously, we have discussed the issues that surround making the diagnosis of pneumonia. We have also touched on some complications and interesting pediatric findings. Additionally, we covered the basic recommended therapies. While the recommendations are for narrow spectrum antibiotics as 1st line (penicillin), many of us still see a lot of broad spectrum antibiotics being used, particularly for those who we admit to the hospital. While it may be fun to say “Cef-Kill-it-All,” is that the right answer for community acquired pneumonia in children?
Community Acquired Pneumonia Basics
- We see a lot of it – accounts for >500,000 ED visits annually!
- Accounts for ~7% of pediatric admissions.
- Streptococcus pneumoniae is the most common bacterial cause of community acquired pneumonia in kids.
- Narrow spectrum beta-lactam antibiotics are still very effective against S. pneumoniae.
- A significant amount of patients (even after published recommendations) continue to receive unnecessary broad spectrum antibiotics as initial therapy!
Penicillin Works Great!
- Several recent studies (see references) support the fact that narrow spectrum antibiotics for community acquired pneumonia is an effective 1st line option.
- Penicillin/Ampicillin/Amoxicillin treat uncomplicated community acquired pneumonia as effectively as broad spectrum agents.
- Broad spectrum antibiotics also work, but increase risk for developing resistant organisms! (Oh, Darwin!)
- S. pneumoniae is the primary target.
- Narrow spectrum penicillins provide appropriate coverage for this bug!
- S. pneumoniae can become resistant to penicillin; however, this is generally a more important consideration for CNS infections (not pneumonia).
- This is true even for those that you are admitting to the hospital!
- The adage “Go Big or Go Home,” does not apply to the selection of 1st line antibiotics for community acquired pneumonia!
- Even if your patient is not going home… you still don’t need to use the “big gun.”
- If they are not responding within 48 hours, then the decision to change therapies can be made.
The Therapeutic Recommendations
- In 2011, the Pediatric Infectious Diseases Society and the Infectious Disease Society of America published guidelines for management of community acquired pneumonia.
-
OutPatient
- Pre-School Age and Fully Immunized
- 1st Line Therapy – Penicillin or Amoxicillin.
- Honestly, the majority are viral pathogens.
- School Age and Fully Immunized
- 1st line therapy = Penicillin or Amoxicillin.
- Consider Atypical Pathogens
- Pre-School Age and Fully Immunized
-
InPatient
- Fully Immunized Infants – School Aged Kids
- If local epidemiologic data does not show high level of penicillin resistance, then
- Ampicillin or Penicillin G
- If local epidemiologic data shows high level of penicillin resistance, then
- 3rd Generation Cephalosporin (ceftriaxone or cefotaxime)
- Consider Macrolide for Atypical Pathogens
- If local epidemiologic data does not show high level of penicillin resistance, then
- Not Fully Immunized or with Life-Threatening Infections (ex, Empyema)
- 3rd Generation Cephalosporin (ceftriaxone or cefotaxime)
- Vancomycin has not been shown to be more effective for empiric therapy in North America.
- Vancomycin or Clindamycin should be consider if infection is consistent with S. aureus.
- Fully Immunized Infants – School Aged Kids
Moral of the Morsel
Obviously, selection of antibiotics for patients needs to be tailored to the specific individual patient (are they immunocompromised, do they have prior history of resistant organisms, are they not vaccinated, etc); however, the decision to admit the patient does not then mandate that the patient receive broad spectrum antibiotics. Good old fashion penicillins are appropriate initial selections for the patient with uncomplicated community acquired pneumonia – whether admitted or discharged.


[…] week we discussed the value of the tried and trusted antibiotic, Penicillin, for pneumonia. In the past we have also mentioned Acute Rheumatic Fever and the management of Strep […]
[…] course, that sounds like pneumonia […]