Posterior Reversible Encephalopathy Syndrome in Children
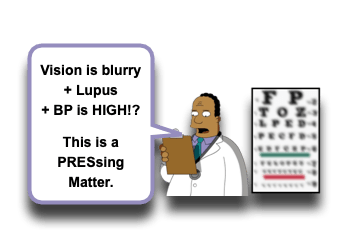
2020! What a great year to focus on good clinical vision! Obviously, in children, what we most often see is, fortunately, the benign conditions; however, it takes our vigilant vision to spot the unusual to help us avoid the life threatening. We have previously discussed some entities that can obscure a child’s vision (ex, Glaucoma, Orbital Cellulitis, Facial Trauma, Multiple Sclerosis, Neonatal Conjunctivitis), but let us now focus on one that can affect their vision and can be easily hidden from our view if we are not attentive (did I take the 2020 vision theme too far? … too bad that wasn’t one of my New Year’s Resolutions) – Posterior Reversible Encephalopathy Syndrome:
Posterior Reversible Encephalopathy Syndrome (PRES)
- Posterior Reversible Encephalopathy Syndrome (PRES) is rare, but does occur in children! [Ghali, 2019; Fisler, 2019]
- True incidence is not really known.
- Really has only been on the diagnostic radar since 1996…
- Most recent estimates have incidence at 0.04% of all hospitalized children. [Thavamani, 2019]
- It is more common in adults… but, children tend to have more multi-organ failure associated with it. [Habetz, 2016]
- True incidence is not really known.
- PRES is diagnosed based on Clinical Features AND Radiologic Findings and the eventual fact of it being Reversible. [Ghali, 2019; Fisler, 2019]
- Clinical Features of PRES: [Ghali, 2019]
- Headache (~58% of cases)
- Altered Mental Status / Confusion (~42% of cases)
- Seizures (~94% of cases)
- Hypertension
- Blurred Vision / Change in Vision (ex, Diplopia) (~16% of cases)
- Visual Field Deficits
- Hemiparesis or Hemianesthesia
- Ataxia, Tremor, Dysmetria, or Dysdiadochokinesia
- Cranial Nerve abnormalities
- Radiologic Findings of PRES: [Ghali, 2019; Gupta, 2016]
- T2-weighted and FLAIR MRI sequences show Vasogenic Edema (regions of hyper-intensity).
- Characteristically is a disease of the supratentorial posterior circulation – and the posterior cortex.
- Has also been shown to affect the frontal and temporal regions.
- Rarely affects posterior fossa.
- Reversibility of PRES: [Ghali, 2019]
- It is important to evaluate other competing conditions on the Ddx, as PRES is essentially defined once it improves… and the others may not improve.
- Typically resolves WITHOUT lasting sequelae.
- Complete resolution occurs in ~90% of cases.
- Symptoms often resolve within first 48 hours of treatment.
- Can RECUR! Those that have recurrence have greater risk for lasting morbidity.
- PRES is associated with increased resource utilization and high risk for morbidity and mortality. [Thavamani, 2019; Fisler, 2019]
PRES Proposed Pathophysiology
- There is yet to be a complete understanding of the pathophysiologic process responsible for PRES, but several theories are based on the following: [Ghali, 2019]
- Disruption of the cerebrovascular auto-regulation resulting in Vasogenic Edema, Hypoperfusion, and Ischemia. [Ghali, 2019]
- Often involves some combination of the following: [Ghali, 2019]
- Hypertension (may be cause of or consequence of)
- Vasoconstriction
- Endothelial dysfunction from:
- Hypertension
- Direct chemotherapeutic endothelial cytoxicity
- Other causes of increased endothelial permeability
- Posterior circulations seem to be most at risk, due to lower protective factors against dysregulation of auto-regulation.
- Conditions that can lead to or exacerbate these conditions can contribute to the development of PRES. [Ghali, 2019]
PRES Risk Factors
- Known to occur in patients with conditions that increase risk for endothelial dysfunction.
- Leading associated conditions are: [Thavamani, 2019; Darwish, 2019; Fisler, 2019; Navarro, 2018; Nasri, 2016]
- Renal Insufficiency (highest risk factor)
- Hypertension
- Malignancies (particularly Leukemia)
- Cytotoxic medications
- Immunosuppressant medications
- Solid Organ Transplantation
- Bone Marrow Transplantation
- Connective Tissue Disorders (ex, Lupus, Scleroderma)
- Sickle Cell Anemia
- Primary Immunodeficiency
- Blood Transfusion
- Severe Sepsis
- Hypomagnesemia
- Anemia
PRES Management
- The primary management of PRES is supportive care. [Ghali, 2019]
- Stop offending agents!
- Antihypertensive therapy
- Antiepileptic therapy
- Valproic Acid and Clonazepam are preferred.
- Phenytoin, carbamazepine, and Phenobarbital should be avoided.
- Therapy continued for 3-12 months for seizure prophylaxis… longer if EEG is abnormal.
Moral of the Morsel
- Altered Mental Status has a wide Ddx! Keep PRES on it!
- Cancer therapy and altered mental status? Think PRES!
- Renal Disease and altered mental status or headache? Think PRES!
- Autoimmune disorder and change in vision? Think PRES!
References
Darwish AH1. Posterior Reversible Encephalopathy Syndrome in Children:: A Prospective Follow-up Study. J Child Neurol. 2020 Jan;35(1):55-62. PMID: 31570037. [PubMed] [Read by QxMD]
Fisler G1, Monty MA2, Kohn N3, Assaad P4, Trope R5, Kessel A5. Characteristics and Outcomes of Critically Ill Pediatric Patients with Posterior Reversible Encephalopathy Syndrome. Neurocrit Care. 2019 May 8. PMID: 31069660. [PubMed] [Read by QxMD]
Anastasopoulou S1, Eriksson MA1, Heyman M1, Wang C1, Niinimäki R2, Mikkel S3, Vaitkevičienė GE4, Johannsdottir IM5, Myrberg IH6, Jonsson OG7, Als-Nielsen B8, Schmiegelow K8, Banerjee J9, Harila-Saari A10, Ranta S1. Posterior reversible encephalopathy syndrome in children with acute lymphoblastic leukemia: Clinical characteristics, risk factors, course, and outcome of disease. Pediatr Blood Cancer. 2019 May;66(5):e27594. PMID: 30592147. [PubMed] [Read by QxMD]
Acar S1, Kavlak ME2, Demir B3, Ozkan P4, Polat KY5, Akyildiz M6, Arikan C7. Posterior Reversible Encephalopathy Syndrome in a Five-Year-Old Child: A Case Report. Transplant Proc. 2019 Sep;51(7):2495-2497. PMID: 31351771. [PubMed] [Read by QxMD]
Ghali MGZ1,2, Davanzo J2, Leo M2, Rizk E2. Posterior reversible encephalopathy syndrome in pediatric patients: pathophysiology, diagnosis, and management. Leuk Lymphoma. 2019 Oct;60(10):2365-2372. PMID: 31556774. [PubMed] [Read by QxMD]
Thavamani A1, Umapathi KK2, Puliyel M3, Super D4, Allareddy V5, Ghori A1. Epidemiology, Comorbidities, and Outcomes of Posterior Reversible Encephalopathy Syndrome in Children in the United States. Pediatr Neurol. 2019 Jul 22. PMID: 31481327. [PubMed] [Read by QxMD]
Komori A1, Mizu D1, Ariyoshi K1. Posterior Reversible Encephalopathy Syndrome: A Rare Childhood Case with Unconsciousness. J Emerg Med. 2018 Apr;54(4):540-543. PMID: 29338905. [PubMed] [Read by QxMD]
Navarro CE1, Rodríguez PJ2, Espitia OM3. Fludarabine-Induced Posterior Reversible Encephalopathy Syndrome in a Pediatric Patient With β-Thalassemia: Case Report and Literature Review. Clin Neuropharmacol. 2018 Nov/Dec;41(6):224-229. PMID: 30273191. [PubMed] [Read by QxMD]
Gupta V1, Bhatia V2, Khandelwal N2, Singh P2, Singhi P3. Imaging Findings in Pediatric Posterior Reversible Encephalopathy Syndrome (PRES): 5 Years of Experience From a Tertiary Care Center in India. J Child Neurol. 2016 Aug;31(9):1166-73. PMID: 27071468. [PubMed] [Read by QxMD]
González Quarante LH1,2, Mena-Bernal JH3, Martín BP3, Ramírez Carrasco M3, Muñoz Casado MJ3, Martínez de Aragón A4, de las Heras RS5. Posterior reversible encephalopathy syndrome (PRES): a rare condition after resection of posterior fossa tumors: two new cases and review of the literature. Childs Nerv Syst. 2016 May;32(5):857-63. PMID: 26584552. [PubMed] [Read by QxMD]
Habetz K1, Ramakrishnaiah R2, Raina SK3, Fitzgerald RT2, Hinduja A4. Posterior Reversible Encephalopathy Syndrome: A Comparative Study of Pediatric Versus Adult Patients. Pediatr Neurol. 2016 Dec;65:45-51. PMID: 27720711. [PubMed] [Read by QxMD]
Nasri A1, Bedoui I2, Mrissa R2, Riahi A2, Derbali H2, Zaouali J2, Messelmani M2, Mansour M2. Recurrent status epilepticus in posterior reversible encephalopathy syndrome as initial feature of pediatric lupus: A newly diagnosed case and literature review. Brain Dev. 2016 Oct;38(9):835-41. PMID: 27068876. [PubMed] [Read by QxMD]
Yamamoto H1, Natsume J2, Kidokoro H2, Ishihara N2, Suzuki M3, Tsuji T4, Kubota T5, Yamada A6, Ozeki M7, Kato Z7, Kawamura Y8, Yoshikawa T8, Okumura A9, Ando N10, Saitoh S10, Takahashi Y2, Watanabe K2, Kojima S2. Clinical and neuroimaging findings in children with posterior reversible encephalopathy syndrome. Eur J Paediatr Neurol. 2015 Nov;19(6):672-8. PMID: 26232050. [PubMed] [Read by QxMD]

