Propofol Infusion Syndrome in Children
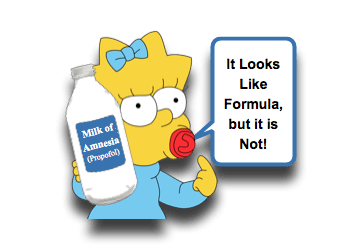 Keeping children calm and cooperative is part of our job and often leads us to using fancy medicines like Ketamine and Nitrous Oxide. Of course, it is important to have a patient safely sedated during a minor procedure like Lumbar Puncture, Facial Laceration Repair, or Incision and Drainage; however, it is even more imperative having just intubating a child. Aside from Ketamine (my favorite drug – professionally speaking), Propofol is one of the most often used tools to keep patients sedated, but our use of it in the ED can occasionally lead to some consternation amongst our friends in the PICU. The reason: concern for mortality! Let us take a minute to digest a Morsel on this important consideration- Propofol Infusion Syndrome:
Keeping children calm and cooperative is part of our job and often leads us to using fancy medicines like Ketamine and Nitrous Oxide. Of course, it is important to have a patient safely sedated during a minor procedure like Lumbar Puncture, Facial Laceration Repair, or Incision and Drainage; however, it is even more imperative having just intubating a child. Aside from Ketamine (my favorite drug – professionally speaking), Propofol is one of the most often used tools to keep patients sedated, but our use of it in the ED can occasionally lead to some consternation amongst our friends in the PICU. The reason: concern for mortality! Let us take a minute to digest a Morsel on this important consideration- Propofol Infusion Syndrome:
Propofol Basics
- First developed in 1973 (not THAT long ago) in the United Kingdom
- Chemically described as 2,6-diisopopylphenol. [Chidambaran, 2015]
- Insoluble in water; must be in oil-in-water emulsion
- Has pKa of 11.
- Propofol works via activation of central GABA pathways and inhibition of NMDA pathways. [Chidambaran, 2015; Diedrich, 2011]
- Propofol Efficacy and Usage:
- Propofol exhibits many pharmacologic advantages:
- Rapid onset
- Short duration
- Few side effects (especially post-anesthetic nausea)
- It is also known to be safe and effectively when administered for procedural sedations inside and outside of the OR. [Kang, 2018; Chidambaran, 2015; Chiaretti, 2014; Rajasekaran, 2014; Vespasiano, 2007; Wheeler, 2003]
- Used for IV induction and Maintenance for General Anesthesia in children. [Kang, 2018]
- FDA approves its use for:
- Maintenance of anesthesia in children 2 months of age and older.
- Induction of anesthesia for children 3 years of age and older.
- Obviously, it is used “off label” beyond these situations.
- FDA approves its use for:
- Commonly used for sedation for short procedures or imaging.
- Propofol is often given with an opioid, as propofol does not address pain from noxious procedures. [Chidambaran, 2015]
- Intermittent bolus administration has greater risk than continuous infusion. [Chidambaran, 2015]
- Propofol has also been safely used in PICUs for RSI and airway management and for short periods at low dosages. [Rosenfeld-Yehoshua, 2016]
- In the ICU, may be used for prolonged sedation. [Chidambaran, 2015; Cornfield, 2002]
- Prolonged use may lead to hypertriglyceridemia and pancreatitis.
- Risk factor for Propofol Infusion Syndrome
- Used for IV induction and Maintenance for General Anesthesia in children. [Kang, 2018]
- Propofol exhibits many pharmacologic advantages:
Problem with Propofol: Propofol Infusion Syndrome
- Adverse reactions can occur with Propofol (just like any medication)
- Pain at injection site – most common side-effect [Chidambaran, 2015]
- Anaphylaxis [Chidambaran, 2015]
- Mitochondrial function depression [Chidambaran, 2015]
- Propofol can uncouple oxidative phosphorylation.
- Mechanism is yet unclear.
- May play role in Propofol Infusion Syndrome.
- “Propofol Infusion Syndrome”:
- Very rare, but deadly complication coincident with Propofol administration.
- True incidence is unknown
- May be an extreme manifestation of a more common and initially reversible physiologic state. [Diedrich, 2011]
- Causation or mechanism has, as yet, not been determined.
- Clinical Features: [Diedrich, 2011]
- Cardiovascular
- Hypotension
- Dysrhythmias (ex, Bradycardia, Wide QRS, Brugada-like ECG, VTach, PEA, asystole)
- Myocardial Failure
- Metabolic
- Hyperthermia
- Metabolic Acidosis
- Renal and Musculoskeletal
- Rhabdomyolysis
- Acute Renal Failure
- Hepatic
- Hepatomegaly and Transaminitis
- Hypertriglyceridemia and Lipdemia
- Cardiovascular
- Very rare, but deadly complication coincident with Propofol administration.
Propofol Infusion Syndrome: Risk Factors
Through evaluation of the case reports and case series, there appears to be several trends for Risk Factors (although, there are also outliers). [Diedrich, 2011; Okamoto, 2003]
- Dose of Propofol >4 mg/kg/hr
- Duration of Propofol 48 hours or greater
- Patients with Inborn Errors of Metabolism
- Concomitant infusion of Vasopressors
- Concomitant use of Steroids
- Patients with “Critical Illness”
- “Younger” Age – although death seemed to more likely occur in patients >18 years of age.
Propofol Infusion Syndrome: Treatment
- There is no specific therapy for Propofol Infusion Syndrome.
- Awareness of it and attempting to prevent it is best option. [Diedrich, 2011]
- Some recommend monitoring serum lactate levels… but, this obviously is not a diagnostic test.
- Maintaining an adequate carbohydrate load to prevent the increase in fatty acids, hopefully reducing risk. [Chidambaran, 2015]
- Propofol Infusion Syndrome is a diagnosis of exclusion!
- The critically ill patient has many reasons to develop the same clinical features.
- Treat all potential etiologies aggressively (ex, sepsis).
- Supportive Care: [Diedrich, 2011]
- Stop the propofol once suspicious for this.
- Improve gas exchange
- Cardiac pacing if bradycardic
- Consider glucagon and phosphodiesterase inhibitors
- Hemodialysis
- ECMO
Moral of the Morsel
- Match your Patients and the Sedatives. As best you are able, consider which medication is right for each specific patient. There is no one perfect medication for everyone.
- Propofol is Powerful. And with great power, comes great responsibility. Use this tool wisely.
- Don’t discount your colleagues’ experience. While we may have not encountered Propofol Infusion Syndrome in the ED, the PICU’s experience may be different.
- Don’t throw the Propofol out with the Bathwater. Over short durations, using appropriate dosages, and in the right patients, the risk of Propofol Infusion Syndrome is likely lower than the risk of the child dislodging the ETT you just placed. Evaluate your risk assessment scales wisely.

