Succinylcholine and the Risk of Pediatric Hyperkalemic Arrest
Intubating a child is a nerve-racking procedure for everyone in the room. We have previously talked about medications (ex, Atropine , Propofol, Ketamine) that are in your toolbox as you prepare for intubation. We have discussed their risks and benefits (Yes, Dr. Fox… Ketamine does have some risks.) As you consider your medication options, selecting the correct paralytic is also imperative. Before you reflexively say “Sux,” we should consider some risks in the pediatric population that come with succinylcholine administration. Let us ponder Succinylcholine and the Risk of Pediatric Hyperkalemic Arrest:
Succinylcholine Basics
- It is a depolarizing neuromuscular blocking agent
- Binds to the nicotinic acetylcholine receptor
- Metabolized by butyrylcholinesterase, which is made in the liver
- Metabolized slower than acetylcholine, which it competitively inhibits
- 10% excreted unmetabolized in urine
- It is on the World Health Organization’s list of essential medicines!
- Succinylcholine Efficacy and Usage: [Alvarellos 2015]
- Succinylcholine exhibits many pharmacologic advantages:
- Rapid onset of action (within 60 seconds)
- Short half-life (duration of action is 4-6 minutes)
- Can use IV or IM
- Great for short procedures that need short term paralysis (which included intubations!)
- Succinylcholine exhibits many pharmacologic advantages:
- FDA approves its use for: [Access Data 2021]
- to facilitate endotracheal intubation
- skeletal muscle relaxation during surgery or mechanical ventilation
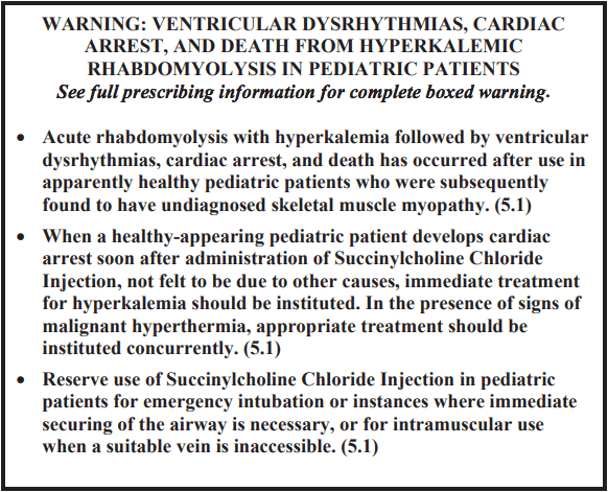
- FDA has put a black box warning on this drug due to cases of rhabdomyolysis leading to hyperkalemic arrest in some pediatric patients.
Succinylcholine: Problems
- Adverse reactions can occur with Succinylcholine (just like any medication)
- The package insert, accessible on the FDA’s Access Data website, specifically indicates the following that have been reported:
- Cardiac arrest
- Malignant hyperthermia
- Arrhythmias
- Bradycardia
- Tachycardia
- Hypertension
- Hypotension
- Hyperkalemia
- Prolonged respiratory depression or apnea
- Anaphylaxis
- Succinylcholine is contraindicated in patients with
- Skeletal muscle myopathies
- Known hypersensitivity to succinylcholine
- After the acute phase of major burns, multi-trauma, denervation of skeletal muscles, or upper motor neuron injury
- History of malignant hyperthermia (personal or family)
Succinylcholine and Hyperkalemia / Hyperkalemic Arrest: Case Reports
Through evaluation of the case reports and case series, there appears to be several trends for Risk Factors (although, there are also outliers).
- Malignant hyperthermia (MH) was first described in Australia 1960. [Alvarellos 2015]
- Mechanism by which succinylcholine induces MH is unknown
- It can trigger MH when administered alone
- Most cases occur when administered with inhalational agent
- Larach et al (1997) reported first cases of hyperkalemic arrest were sent to the Malignant Hyperthermia Association of the United States in 1992 Data from 1990-1993 in pediatric arrests after anesthesia
- All had pre-op evaluation and were normal and healthy
- 72% received succinylcholine
- 25 patients arrested, mean K+ level 7.4, hyperkalemia in 72%
- Undiagnosed Duchenne muscular dystrophy or myopathy in 48%
- Recommended a screening creatine kinase for myopathy in males before anesthesia
- Rosenberg et al (1992) described four males under 8 years who received halothane and succinylcholine with subsequent massive rhabdomyolysis and hyperkalemia leading to arrest and death.
- Sullivan et al (1994) reported two healthy pediatric patients
- One with wide complex ventricular tachycardia
- One with asystolic arrest
- Both found to have dystrophin-deficient muscular dystrophies (Duchenne and Becker, respectively)
- Parker et al (1995) reported an 8 mo male with myringotomy tube removal and adenoidectomy intubated with succinylcholine
- Had a 13 minute cardiac arrest with maximum K+ of >10.
- Found to have red urine and a creatine kinase level of 280,000 U/L (normal <200 U/L)
- Subsequently diagnosed with Duchenne muscular dystrophy
- Piotrowski (2007) described a 16 yo with leukemia and sepsis
- Required reintubation after first use of succinylcholine was uneventful
- Second dose caused potassium rise from 3.19 to 8.64 mmol/L
- Suffered cardiac arrest but was resuscitated
- Hyperkalemia resolved in 30 minutes
Hyperkalemia and Hyperkalemic Arrest: Risk Factors
The mechanism of life-threatening arrhythmias and arrest was proposed by Rosenberg et al to be massive rhabdomyolysis (from depolarizing effects of succinylcholine) leading to acute hyperkalemia, which precipitates wide complex tachyarrhythmias, bradyarrhythmias, and arrest. [Rosenberg 1992, Sullivan 1994]
Risk Factors to be considered:
- Younger males with potential for undiagnosed muscular dystrophies
- Undiagnosed dystrophin gene disorders
- Patients with unknown medical history or down time
- Subacute multi-trauma
- Subacute major burns
- Family history of malignant hyperthermia
Rhabdomyolysis, Hyperkalemia, and Hyperkalemic Arrest: Treatment
- Calcium Chloride can provide cardiac stabilization in hyperkalemia
- Glucose and insulin can treat hyperkalemia quickly
- Dantrolene may be of use when malignant hyperthermia is on the differential [Rosenberg 1992]
- Rhabdomyolysis should be aggressively treated with IV hydration and monitoring for renal function.
Can I Use Succinylcholine in Pediatric Patients?
- Yes, the FDA still approves of succinylcholine for emergent endotracheal intubation. [Lafferty 2019]
- BUT… Realize the risk of serious side effects, especially in young children, in males, and in those with unknown medical histories
- You have other options! [Joseph 2019]
- Joseph et al put Succinylcholine head to head with Rocuronium
- Cost: rocuronium $40/100mg vial- shelf stable for 12 weeks. Succinylcholine $40/200mg vial, but only shelf stable for 2 weeks.
- Onset time: Same duration of 45-60 seconds when the higher end dose of rocuronium is used (1.2 mg/kg)
- Rocuronium has a limited side effect profile, mostly hepatoxicity, compared to long side effect profile of succinylcholine
- Chance for first past success: It’s a draw! Both are effective.
- Duration: rocuronium lasts 30-90 minutes where succinylcholine lasts 10-15 minutes.
- We now have a reversal agent for Rocuronium (Sugammadex) if you need shorter paralysis.
- (Although, Dr. Fox says that he has yet to meet a patient that he decided needed to be intubated that he wanted to the paralytic to wear off quickly in).
Moral of the Morsel
- Match your patients and the paralytic. Consider using alternatives to succinylcholine for your younger patients, especially males.
- No drug is perfect. Know the side effect profile, the adverse reactions and events, and how to treat them, no matter which drug you choose.
- It may paralyze AND ALSO injure the muscles in some! Succinylcholine may cause rhabdomyolysis in some children leading to hyperkalemia and subsequent arrest.
- Don’t throw the Succinylcholine out with the Bathwater. It can still be safely used in some pediatric patients, and is a drug with some benefits, in the correct patient populations.
References
- Joseph, DO, EMT, J., DiCorpo, BSC, MMSc, PA, J., Rice, MD, MICP, D., Merlin, DO, EMT-P, FACEP, M. and Weber, MD, EMT, A., 2019. Succinylcholine vs. Rocuronium: Battle of the RSI Paralytics. [online] Available at: <https://www.jems.com/patient-care/succinylcholine-vs-rocuronium-battle-of-the-rsi-paralytics/> [Accessed 3 December 2021].
- Tyson J. Olds, George R. Kracke; Nobel Prize for Anesthesia Pioneer. Anesthesiology 2017; 126:354 doi: https://doi.org/10.1097/ALN.0000000000001453
- https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/215143s000lbl.pdf. Published 2021. Accessed December 3, 2021.
- Alvarellos ML, McDonagh EM, Patel S, McLeod HL, Altman RB, Klein TE. PharmGKB summary: succinylcholine pathway, pharmacokinetics/pharmacodynamics. Pharmacogenet Genomics. 2015;25(12):622-630. doi:10.1097/FPC.0000000000000170
- Larach M, Rosenberg H, Gronert G, Allen G. Hyperkalemic cardiac arrest during anesthesia in infants and children with occult myopathies. Hyperkalemic cardiac arrest during anesthesia in infants and children with occult myopathies | Meta. https://www.meta.org/papers/hyperkalemic-cardiac-arrest-during-anesthesia-in/9007342. Published 1997. Accessed December 3, 2021.
- Rosenberg, H., Gerald, 1992. Intractable Cardiac Arrest in Children Given Succinylcholine. Anesthesiology 77, 1054–1054.. doi:10.1097/00000542-199211000-00040
- Sullivan, M., Thompson, W.K., Hill, G.D., 1994. Succinylcholine-induced cardiac arrest in children with undiagnosed myopathy. Canadian Journal of Anesthesia/Journal canadien d’anesthésie 41, 497–501.. doi:10.1007/bf03011544
- Parker, Steven F. MD; Bailey, Ann MD; Drake, Amelia F. MD Infant Hyperkalemic Arrest After Succinylcholine, Anesthesia & Analgesia: January 1995 – Volume 80 – Issue 1 – p 206-207
- Piotrowski, Andrzej & Fendler, Wojciech. (2007). Hyperkalemia and cardiac arrest following succinylcholine administration in a 16-year-old boy with acute nonlymphoblastic leukemia and sepsis. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 8. 183-5. 10.1097/01.PCC.0000257103.96579.B2.
- 4. Lafferty MD K, Windle, PharmD M, Dillinger R. Which patients are at risk for succinylcholine-induced hyperkalemia during tracheal intubation?. Medscape.com. https://www.medscape.com/answers/109739-91185/which-patients-are-at-risk-for-succinylcholine-induced-hyperkalemia-during-tracheal-intubation. Published 2019. Accessed December 3, 2021.

