Pleural Effusion and ReExpansion Pulmonary Edema
Pleural Effusion: Basics
- Pleural effusion = fluid accumulation in pleural space.
- Occur at ANY AGE … even neonates! [Lee, 2018]
- Occur when rate of absorption < rate of accumulation
- Factors that influence development of pleural effusion: [Lee, 2018]
- Hydrostatic Pressure
- Oncotic Pressure
- Lymphatic Pressure
- Regional Inflammation
- Clinical presentation of pleural effusions depends on size of effusion and any associated medical conditions/causes.
Pleural Effusion: Causes
- There are numerous causes!
- Anything that affects the factors noted above can lead to pleural effusion.
- Often individual causes influence development via multiple factors.
- Infection is the leading identified cause of pleural effusions. [Utine, 2009]
- Parapneumonic Effusion accounted for ~78% of cases in one study. [Utine, 2009]
- Tuberculous is a notable cause as well. [Utine, 2009]
- Malignant Effusions accounted for ~4% of cases. [Baniak, 2017; Utine, 2009]
- Congenital Heart Diseases accounted for ~1% [Utine, 2009]
- Chylothorax accounted for <1% of cases. [Utine, 2009]
- Many causes go Unidentified. [Utine, 2009]
- Acquired or Iatrogenic pleural effusions occur TWICE as often as congenital effusions. [Lee, 2018]
Pleural Effusion: Management
- Imaging:
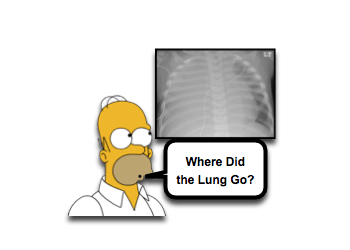
- CXR is often first image obtained and may show:
- Fluid in fissures
- Blunting of costophrenic angle
- Mass effect
- Meniscus formation
- Ultrasound should be considered early!
- It is timely and “easy” to do at the bedside …
- So sick child doesn’t have to leave your department
- Check out video at bottom of this page (and on mededmasters.com)
- Can detect smaller volumes of effusion than CXR.
- It is timely and “easy” to do at the bedside …
- CT may be useful in evaluation, but not until patient is clinically stable.
- May help show associated anatomic abnormality or cause (ex, migrated VP shunt tip). [Porcaro, 2018]
- May show associated traumatic injuries (if effusion related to trauma). [Kulaylat, 2014]
- CXR is often first image obtained and may show:
- Drainage / Thoracentesis:
- Small bore catheters are generally favored over large calibre tubes.
- Better tolerated.
- Less complication risk.
- Do the job!
- See Morsel on Pigtails Catheters.
- SMALL Asymptomatic pleural effusions may resolve with treatment aimed at underlying condition.
- Medical Management may include:
- Specialty nutrition with high medium-chain triglyceride content (decreases intestinal lymph production and decreases flow through thoracic duct).
- Octreotide may reduce need for surgical intervention.
- Treat underlying issue:
- If related to uremia – initiation of hemodialysis. [McGraw, 2017]
- If central line in place, remove as it may be causing obstruction. [Lee, 2018; Siddiqui, 2015]
- Medical Management may include:
- Small bore catheters are generally favored over large calibre tubes.
- Characterize Pleural Fluid:
- Samples of pleural fluid should be sent for: [Lee, 2018]
- pH
- Cell Count
- Gram Stain and Culture
- Protein
- Glucose
- Lactate Dehydrogenase
- Triglycerides
- Transudative vs. Exudative Process [Lee, 2018]
- Exudative effusion tend to have:
- Cloudy appearance
- Specific gravity > 1.020
- Elevated protein
- Lactate dehydrogenase levels > 2/3rds the serum level
- Transudative effusion tend to have:
- Clear appearance
- Specific gravity < 1.012
- Protein level < 2.5 g/dL
- Fluid Protein: Serum Protein < 0.5
- Lactate dehydrogenase level < 2/3rds the serum level
- Light’s Criteria is often used to help classify pleural fluid, although it hasn’t been validated in children. [McGraw, 2018; Less, 2018]
- Exudative effusion tend to have:
- Samples of pleural fluid should be sent for: [Lee, 2018]
ReExpansion Pulmonary Edema
- Reexpansion Pulmonary Edema is uncommon, but can occur AFTER expansion of a collapsed lung.
- Most commonly described in the setting of treatment of Pneumothorax or Pleural Effusion. [Hirsch, 2018]
- Risk Factors: [Hirsch, 2018]
- There is no clear evidence to attribute any specific risk factor for development of Reexpansion Pulmonary Edema in children.
- Some considerations though are:
- Younger age
- Use of high suction pressure (recommended to use between -10 to -20 cmH2O, or even just water seal at first).
- Chronically collapsed lung
- Larger size of Pneumothorax or Pleural Effusion
- In the end, Reexpansion Pulmonary Edema can occur in a variety of situations and requires vigilance.
- Presentation: [Hirsch, 2018]
- May be asymptomatic (only seen on repeat imaging)
- Tachypnea, worsening dyspnea
- Cough, sometimes productive with pink frothy sputum
Moral of the Morsel
- Be Kind! Use a pigtail catheter to drain effusion.
- Characterize the Fluid! Light’s Criteria may help distinguish exudative from transudative, but nothing is perfect.
- Don’t ignore that cough! After placement of the pigtail catheter, don’t just assume all will be fine. Monitor for Reexpansion Pulmonary Edema.

