Urinary Retention in Kids
Urinary Retention: Basics
- Urinary retention is uncommon in children.
- It is defined as a volume of retained urine > expected bladder capacity
- Estimated Bladder Capacity in Ounces = Age in years + 2 [Gatti, 2001; Peter, 1993]
- Remember Fluid Ounce = ~ 30 mL
- Not defined by duration from last urination
- May reflect other issues, like dehydration.
- Estimated Bladder Capacity in Ounces = Age in years + 2 [Gatti, 2001; Peter, 1993]
- Child may present with:
- Dribbling or urine
- Weak stream
- Unable to initiate bladder emptying
- Abdominal pain
- Palpable abdominal mass (bladder above pubic bone)
Urinary Retention: Causes in Kids
- Infection
- One of the most common causes [Peter, 1993]
- Examples: Cystitis, Pyelonephritis
- Systemic viral illnesses also implicated (ex, adenovirus, EBV) [Chu, 2013; Gatti, 2001]
- Neuromuscular Dysfunction
- Are a prevalent cause in children. [Gatti, 2001]
- Acute Disseminated Encephalitis (ADEM) [Burla, 2016]
- Presents with paresthesias, paralysis, ataxia, vision changes, and/or altered mental status.
- Often preceded by viral illness or vaccine administration.
- Other examples: Guillain-Barre Syndrome, Multiple Sclerosis, Transverse Myelitis, Spina Bifida, Tethered cord [Burla, 2016; Gatti, 2001; Peter, 1993]
- Congenital Obstructive Lesions
- Examples: Posterior urethral valves, Polyps [Peter, 1993]
- Constipation
- Yup… that is a lot of stool!
- Thought to be due to marked elevation of the bladder floor and posterior urethra by the distended rectum. [Gatti, 2001; Peter, 1993]
- Medications
- Adverse drug effects are very commonly implicated. [Gatti, 2001]
- ex, Cold medications, antihistamines, neuroleptics, alpha-adrenergic agonists
- Postoperative
- Renal Stones
- Misc.
- Hypermagnesemia (newborn exposed to maternal Magnesium)
- Voluntary overdistention [Peter, 1993]
- Potty training may lead to avoiding urination, leading to increased bladder volume.
- Stretching of the bladder beyond its normal capacity impairs its elastic properties and can hinder voiding.
- Pelvic masses [Binder, 2015; Gatti, 2001]
- Local inflammatory processes [Gatti, 2001]
- Meatal stenosis, balanoposthitis, labial adhesions
- Peri-apendiceal Abscess [Parrish, 1993]
- Incarcerated inguinal hernia [Gatti, 2001]
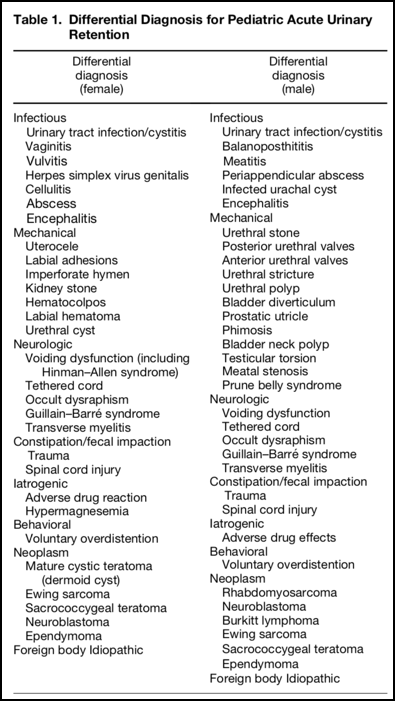
- See Table 1 below, courtesy of Binder et al., 2015
Urinary Retention: Management
- Drain the bladder!
- If the belief is that the cause is temporary (ex, constipation, voluntary overdistention), then may consider in-and-out cath to decompress bladder.
- If unsure, or concern for other neurologic condition, place foley.
- If not using a foley, patient will need to demonstrate ability to void on her/his own before discharge.
- Children with UTIs may be instructed to soak in bath of warm water to help with urination (obviously, this is at their home… not your ED).
- Check for infection!
- This is a prevalent cause, so don’t overlook UTI.
- At the same time, don’t be too eager to diagnose UTI and overlook other more ominous signs.
- Perform a thorough Neuro Exam!
- Of greatest concern – is there a spinal cord or other neurologic condition that is the cause?
- Inspect the back carefully… look for evidence of occult spinal abnormalities.
- If a clear reason is not obvious, have a low threshold for considering spinal imaging. [Gatti, 2001]
- What’s the Anatomy?
- Even those who have a UTI, may have it because of an anatomic abnormality.
- Consider Ultrasound:
- Evaluate for hydronephrosis
- Evaluate for masses
- If not getting U/S in ED, ensure follow-up to consider imaging.
Moral of the Morsel
- It may be rare, but it does happen. As always, remain vigilant.
- Urinary retention is ominous. Don’t simply send the child home with a foley and a leg bag like you may do for the old gentleman with prostate problems.
Ddx of Urinary Retention
References
Burla MJ1, Benjamin J1. Pediatric Urinary Retention in the Emergency Department: A Concerning Symptom with Etiology Outside the Bladder. J Emerg Med. 2016 Feb;50(2):e53-6. PMID: 26482829. [PubMed] [Read by QxMD]
Binder Z1, Iwata K1, Mojica M2, Ginsburg HB3, Henning J1, Strubel N4, Kahn P5. Acute Urinary Retention Caused by an Ovarian Teratoma-A Unique Pediatric Presentation and Review. J Emerg Med. 2015 Nov;49(5):e139-42. PMID: 26275742. [PubMed] [Read by QxMD]
Heckmann R1, de la Fuente FA1, Heiner JD2. Pediatric urinary retention and constipation: vaginal agenesis with hematometrocolpos. West J Emerg Med. 2015 May;16(3):418-9. PMID: 25987917. [PubMed] [Read by QxMD]
Chu SD1, Singer JS. Acute urinary retention secondary to Epstein-Barr virus infection in a pediatric patient: a case report and review of causes of acute urinary retention in children. Urology. 2013 May;81(5):1064-6. PMID: 23465533. [PubMed] [Read by QxMD]
Gatti JM1, Perez-Brayfield M, Kirsch AJ, Smith EA, Massad HC, Broecker BH. Acute urinary retention in children. J Urol. 2001 Mar;165(3):918-21. PMID: 11176514. [PubMed] [Read by QxMD]
Parrish GA1, Wright GD, Falk JL. Acute urinary retention: an unusual presentation of appendiceal abscess. Ann Emerg Med. 1993 May;22(5):857-60. PMID: 8470845. [PubMed] [Read by QxMD]
Peter JR1, Steinhardt GF. Acute urinary retention in children. Pediatr Emerg Care. 1993 Aug;9(4):205-7. PMID: 8367356. [PubMed] [Read by QxMD]
Nishimoto N, Kajikawa J, Miyoshi S, Iwao N, Mizutani S, Okuyama A. Urinary retention secondary to ovarian dysgerminoma in a girl. Urology. 1985 Jul;26(1):71-3. PMID: 4012986. [PubMed] [Read by QxMD]


Hi Dr Fox,
My son was diagnosed 2 years with paruresis at age 17. He had seen a pediatric urologist who suggested his inability to pee was psychological. The only test performed was a sonogram, which showed he was retaining some urine even after going.
He feels bladder pain when it is full, but can not go unless he is home.
My concern going forward is first, was a physical cause missed? I’ve read up on shy bladder, and I understand that many Americans are affected.
Second, what permanent damage is being done to his body by holding urine for long periods of time on a daily basis? What Dr should be monitoring him and how often should he be evaluated? Currently he is working with a therapist.
As a parent, it’s hard to watch your child go through something so debilitating without being able to offer any help.
Thanks for any advice 🙏 ❤
My child was not passing urine since of one day . And she was age of two years and one week .so what is main caused of it
My son When passing urine have delays to come out. if I asked him get pain or burn feeling he get answer that nothing or no. My I Know any problem for him.
My daughter is with type 1diabetes for about the last month I have been smelling a strong odor from her smells like old pee, I have asked her us she has had a problems and having accidents in her pants or bed wetting she insists that she is not on both of those question I don’t know if she is and is embarrassed to say something but she can be sitting next to me and the smell is so strong what do I do
She is 12 years old
Shannon,
Obviously, I cannot give out individual specific medical advice. That being said, I would advocate for any parent / family who is concerned about a child to reach out to their primary physician to help sort through the potential issues.
Hope all is well,
sean
Hi Sean, my 5 year old has a distended bladder and is now on an open/close catheter. In order to retrain and re-tone the bladder should we empty it every 3 hours or try and wait to see if he feels the need to go? Should we be doing this through the night as well or OK to leave it closed at night as he would normally be?
I cannot give specific medical advice out online. I would encourage you to ask this specific question to your child’s Urologist. I suspect that your Urologist has a specific recommendation about this and I would not want to contradict them.
I hope all resolves soon,
sean
Hi, my child has not passed urine for two days now, she was under cotrimoxazole syrup 3 days ago. The child is 7 months old, with good feeding habit and not irritable. Body weight is 8kg. What should i do
I am sorry that your child isn’t feeling well. Obviously, I cannot give out specific medical advice online… but I will say that it is always best to communicate openly with your medical providers. Inform her/him of your concerns. It sounds like your son may have oral thrush (the medicine he is one is an anti fungal)… and if he is eating well, that is great! Until you speak with your pediatrician, keep feeding your child as usual and monitoring the urine output.
I hope all resolves quickly.
-sean
Thanks for post Sean fox
[…] we discussed Urinary Retention in Kids and highlighted how this is not a condition that only affects adults and the elderly. Obviously, […]
Sean Fox,thank you so for you post. Much thanks again.
My name is Zachary Binder. I am a pediatric emergency medicine fellow at Boston Medical Center. My article: “Acute Urinary Retention Caused by an Ovarian Teratoma-A Unique Pediatric Presentation and Review,” was referenced in your recent article “Urinary Retention in Kids”. I am glad that you found the article useful. Please feel free to use or incorporate “Table 1” from my article in the future. It was created in the hopes that it would be distributed in forums such as this one.
Dr. Binder,
I appreciate that!
(can you send a high resolution version of the table to pedemmorselsfox@gmail.com so I can avoid blurriness that comes with snagging tables from PDFs?)
THANK YOU,
sean