Recurrent Abdominal Pain
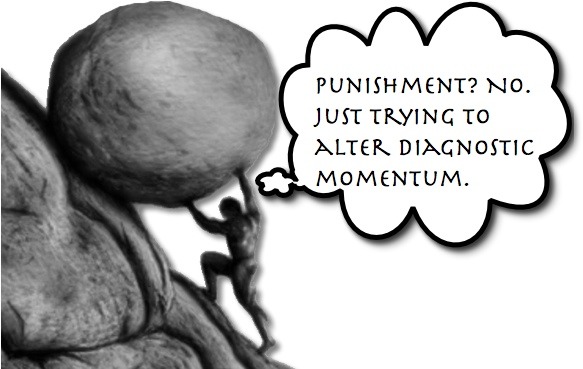
Like Sisyphus, you may feel that you are continually pushing a diagnostic boulder up a mountain only to watch it roll back down. Certainly, some diagnoses offer less of an incline to overcome; however, others, like Chronic Recurrent Abdominal Pain (CRAP), are like the Alps.
Previously, we have discussed various significant etiologies of abdominal pain:
- Intussusception
- Pancreatitis
- Ovarian Torsion
- NEC
- Malrotation
- Kidney Stones
- Cholelithiasis
- Crohn’s Disease
- HSP
- Appendicitis
- Typhlitis
Naturally, with the first encounter of a patient, we are all adept at considering the above potential issues (and numerous others), but the challenge is increased with the patient that presents with similar complaints as previous encounters — particularly when there has been a diagnosis already given, like CONSTIPATION.
A recent publication by a colleague (J Homme) reminded me of how difficult our job can be and how diagnostic momentum may obscure the real diagnosis: especially, when the diagnosis is not one you commonly consider (Ureteropelvic Junction Obstruction).
Chronic Abdominal Pain
- Estimated that 13-17% of the pediatric population has chronic abdominal pain!
- Defined as “long lasting intermittent or constant abdominal pain that is functional or organic.”
- That is pretty broad of a definition.
- Generally, these patients lack serologic, radiographic, mucosal or structural abnormalities.
- There are actually diagnostic criteria that can categorize the conditions (which we won’t go into).
- Many organic conditions can lead to “Chronic Abdominal Pain.”
- ex, Celiac Disease, Inflammatory bowel disease, gallbladder disease, pancreatitis, esophagitis, malignancies, retained foreign bodies, porphyria, food intolerances, lead poisoning, abdominal migraine, etc, etc, etc.
- These are the things that must be considered prior to “labeling the child,” but are often not completely ruled out (common things being common… and zebras, being zebras).
- Functional abdominal pain is the most common cause of chronic abdominal pain.
WAIT! Don’t Stop Reading!!
Ok… I know. None of you want to read about chronic abdominal pain. In fact, I don’t want to write about it, but that is part of the issue. We don’t want to deal with it. So, once the child’s chart says anything about “chronic abdominal pain,” I stop thinking. I may convince myself to consider the absolute emergencies (ex, obstruction, appendicitis) and then say, “I don’t think an emergency is going on. You need to go see your GI doctor.”
While that may be true, remember the boulder of diagnostic momentum may be approaching to crush us. Did this child actually get a thorough evaluation for this previous to our exam? Have all of the terrible things been considered? Is the parent paranoid or correct and we are being callous?
Some Red Flags to Consider
- Family history of GI disease
- Weight Loss
- Oral Ulcers
- Delayed Puberty
- Unexplained Rashes or Joint Pain
- Back/Shoulder/Bone Pain
- Blood in emesis/stool, bilious emesis
- Flank Pain/Hematuria
- Anemia
One to Add to Your DDX:
Ureteropelvic Junction Obstruction
- Most common cause of antenatal and neonatal hydronephrosis
- Can present at any age.
- Intermittent obstruction of the ureter, which can be due to a variety of causes.
- Often difficult to diagnose due to the intermittent nature of it.
- Abdominal pain may be present for years prior to diagnosis.
- Renal Ultrasound is a good first imaging tool, but may be falsely normal.
- The asymptomatic child will likely have normal anatomy during the study.
- Hydration and diuretic administration can improve test performance.
- Contrasted CT – can help, but diuretics also help improve study.
- MAG-3 diuretic scintigraphy is considered the better imaging study.
- Naturally, not a study typically available in the ED.
Moral of the Morsel
Be reluctant to dismiss the child who has been labeled with “chronic abdominal pain” as just having another attack of the non-specific disease. That does NOT mean that you need to order a MAG-3 study on every kid though. What it means is that we reprocess the DDx ourselves and then should speak with empathy to our patients and their families. While reporting that we don’t think there is an emergency going on this time, we should be humble enough to report that there may very well be an organic cause that has yet to be determined… like Ureteropelvic Junction Obstruction.


[…] with abdominal pain or vomiting. While the symptoms may be related to non-emergent etiologies (ex, CRAP, Epiploic Appendagitis), our vigilant minds wrestle with concerns for Intussusception, […]
[…] caring for children, we are all prepared for evaluating abdominal pain as it seems like every condition leads can cause belly pain. Fortunately, this means the odds […]
[…] clinical skills to help benefit a child. To ensure that we don’t disregard the patient with Chronic Recurrent Abdominal Pain so quickly or overlook the significance of Pica, let us review Lead […]